권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
Title Page
Abstract
Contents
List of abbreviations 24
CHAPTER 1. Introduction 28
1.1. Nonthermal atmospheric pressure plasma 29
1.2. Skin Biology 31
1.3. Coronavirus 33
1.4. Objectives of this thesis 35
CHAPTER 2. Periodic exposure of plasma activated medium alters fibroblast cellular homeostasis 37
2.1. Introduction 38
2.2. Materials and methods 40
2.2.1. Cell Culture 40
2.2.2. PAM generation and treatment 40
2.2.3. Cell growth assay 41
2.2.4. Terminal cell death 41
2.2.5. Quantitative real-time PCR analysis 42
2.2.6. Reactive species (RONS) detection 42
2.2.7. Cell Cycle analysis 42
2.2.8. Cell energetics assay (ATP measurement) 43
2.2.9. Flow cytometry for mitochondria membrane potential 43
2.2.10. Confocal microscopy 43
2.2.11. Statistics 43
2.3. Results 44
2.3.1. Physical characteristics of soft jet plasma 44
2.3.2. Single and periodic exposure to PAM leads to reduced viability of fibroblasts 45
2.3.3. PAM exposure increases reactive species accumulation and triggers cellular antioxidant proteins 48
2.3.4. Periodic PAM exposure effect on fibroblast cell energetic 49
2.3.5. Periodic PAM exposure induces the DNA damage response and cell cycle arrest in fibroblast cells 51
2.4. Discussion 53
CHAPTER 3. Influence of redox stress on crosstalk between fibroblasts and keratinocytes 57
3.1. Introduction 58
3.2. Materials and methods 60
3.2.1. Cell Culture 60
3.2.2. Plasma exposure 60
3.2.3. Cellular metabolic viability 61
3.2.4. Measurement of cellular ATP 62
3.2.5. Mitochondria membrane potential 62
3.2.6. Cell migration assay 62
3.2.7. Quantitative PCR (qPCR) analysis 62
3.2.8. Statistics 63
3.3. Results 63
3.3.1. Soft Jet plasma and RONS concentrations 63
3.3.2. GM and HaCaT cell proliferation is enhanced after NTP treatment 64
3.3.3. Low dose plasma enhances the expression of cross talk molecules between fibroblasts and keratinocytes 66
3.3.4. Fibroblast and HaCaT cell migration is enhanced under low plasma conditions 68
3.4. Discussion 70
CHAPTER 4. Identification of nonthermal plasma regulated microRNAs for melanoma inhibition 74
4.1. Introduction 75
4.2. Materials and methods 78
4.2.1. Cell culture 78
4.2.2. Plasma treatment for melanoma system 79
4.2.3. Cell viability 79
4.2.4. Total ATP measurement 79
4.2.5. Flow cytometric analysis for ROS 79
4.2.6. Confocal ROS 79
4.2.7. Melanoma migration 80
4.2.8. Quantitative Real Time Polymerase Chain Reaction (qPCR) 80
4.2.9. RNA seq - Melanoma- miRNA 80
4.2.10. Bioinformatic analysis 81
4.2.11. Statistics 81
4.3. Results 81
4.3.1. Plasma inhibits melanoma cells 81
4.3.2. Plasma reduces cellular energetics 82
4.3.3. Plasma generates ROS 83
4.3.4. Plasma effect on tumorigenesis. 84
4.3.5. High throughput RNA sequencing of miRNAs 85
4.3.6. Identification and validation of candidate miRNAs 85
4.4. Discussion 89
CHAPTER 5. Pulsed 3.5 ㎓ high power microwaves irradiation on physiological solutions and their biological evaluation on human cell lines 92
5.1. Introduction 93
5.2. Materials and Methods 96
5.2.1. HPM exposure system 96
5.2.2. Cell culture 97
5.2.3. Measurement of Nitric oxides (NOx) species in liquid solutions[이미지참조] 97
5.2.4. Measurement of H₂O₂ in liquid solutions 97
5.2.5. Experimental setup 98
5.2.6. Metabolic activity 98
5.2.7. Measurement of intracellular nitric oxide (NO) 98
5.2.8. Cell death analysis by flow cytometry 98
5.2.9. Apoptosis and necrosis assessment 99
5.2.10. Gene expression analysis by quantitative PCR method 99
5.2.11. Statistical analysis 99
5.3. Results 100
5.3.1. Physical properties of the HPM exposure device 100
5.3.2. Preliminary assessment in human cell lines 103
5.3.3. Analysis of cell death by HPM irradiated solutions 106
5.3.4. HPM-irradiated solutions induced transcription of apoptotic genes 108
5.4. Discussion 110
CHAPTER 6. Effect of plasma generated ozone on coronavirus infectivity 113
6.1. Introduction 114
6.2. Materials and methods 117
6.2.1. Cell Culture and Viral strains 117
6.2.2. DBD plasma device and benchtop ozone chamber 118
6.2.3. Experimental procedure 118
6.2.4. Cellular viability assay 119
6.2.5. Infectivity assay 120
6.2.6. Evaluation of viral RNA expression and host cell mRNA expression 120
6.2.7. Viral Integration assay - Immunofluorescence assay 120
6.2.8. Statistics 121
6.3. Results 121
6.3.1. DBD Plasma physical characteristics 121
6.3.1. PGO reduces TCID50 of surface HCoV 229E[이미지참조] 123
6.3.2. Selectivity index of PGO against HCoV-229E in MRC-5 cells 125
6.3.3. PGO reduces HCoV-229E infectivity by inhibiting viral RNA expression and spike glycoprotein levels 126
6.3.4. PGO stimulates host cell antiviral response program 128
6.4. Discussion 129
CHAPTER 7. Summary and Future Scope 133
7.1. Summary 134
7.2. Future scope 135
References 137
Appendix 171
Appendix 1. List of primer sequences used in this thesis 171
Appendix 2. Protocol for stock preparation of coronaviruses (HCoV-229E) 174
Appendix 3. Protocol for determination of HCoV-229E viral titer 174
Appendix 4. Calculation of viral titer - TCID50[이미지참조] 174
Curriculum Vitae 177
Figure 1.1. Plasma as fourth state of matter. 29
Figure 1.2. Factors affecting interactions between plasma and its target 30
Figure 1.3. Plasma device types and reactive species. (a) volume dielectric barrier discharge... 30
Figure 1.4. Nonthermal plasma application potential in skin biology 32
Figure 1.5. Coronavirus cases burden globally as of November 26th, 2021.[이미지참조] 34
Figure 1.6. Classification of the coronaviruses 34
Figure 2.1. Types of skin cells in different layers of the skin 38
Figure 2.2. Standardization of PAM for treatment 41
Figure 2.3. Description of Soft jet plasma used in this study. a) Schematic representation of... 44
Figure 2.4. Physical characteristics of soft jet plasma. (a) Optical emission spectrum of the... 45
Figure 2.5. Schematic representation of study and experimental plan 45
Figure 2.6. Effect of periodic exposure of PAM on cell survival. (a) Representative graph... 46
Figure 2.7. Gene expression data as measured by qPCR for (a) Casp3, (b) Casp8 (c) Casp9... 47
Figure 2.8. Measurement of total ROS after PAM exposure. (a) Relative concentration of... 48
Figure 2.9. Gene expression profile of antioxidant enzymes (a) GPx, (b) catalase (c)... 49
Figure 2.10. Effect of PAM on cellular energetics. (a) ATP levels in fibroblast cells exposed... 50
Figure 2.11. Evaluation of mitochondrial membrane potential. Mitoflow intensity levels in... 50
Figure 2.12. Cell cycle analysis of fibroblasts after PAM exposure. (a) Representative cell... 51
Figure 2.13. Assessement of DNA damage and DNA damage responses. (a) Representative... 52
Figure 3.1. Fibroblast and keratinocytes interactions 59
Figure 3.2. In vitro 3D Co-culture model. Fibroblasts (GM) cultured at bottom part of well... 61
Figure 3.3. Measurement of reactive species and pH. (a) H₂O₂ concentration in medium. (b)... 63
Figure 3.4. Effect of plasma exposure on metabolic activity and cellular energetics. (a)... 65
Figure 3.5. Effect of plasma on proliferation and mitochondrial health of fibroblasts and... 66
Figure 3.6. Gene expression quantified using qPCR for (a) KGF (b) MMP2 (c) GM-CSF (d)... 67
Figure 3.7. Effect of plasma exposure on migration potential. (a) Cell migration assay in co-... 69
Figure 3.8. Gene expression profile of (a) YAP, (b) CYR61, and (c) CTGF were measured... 70
Figure 4.1. An illustration depicting malignant transformation of melanocytes 75
Figure 4.2. miRNA biogenesis and its putative functions 76
Figure 4.3. Reported functions of known miRNAs in various cellular biological processes... 77
Figure 4.4. Function of known miRNAs in melanoma progression. 78
Figure 4.5. Cellular viability of melanoma cells (a) SK-2 and (b) SK-31 after exposure to... 81
Figure 4.6. Measurement ATP levels in SK-2 cells. Graph showing levels of (a) intracellular... 82
Figure 4.7. Detection of ROS. (a) qualitative assessment by confocal microscopy and (b)... 83
Figure 4.8. Image showing results of scratch wound assay and associated graph indication... 84
Figure 4.9. Bioinformatic analysis of RNASeq data. (a) Schematic of High throughput RNA... 86
Figure 4.10. Expression validation of candidate miRNAs (a) Bar graph showing top... 87
Figure 4.11. Validation of miRNA expression in G-361 cells (a) graph showing cellular... 88
Figure 5.1. Interaction between plasma and biological cell 93
Figure 5.2. Schematic configuration of the diode part of the HPM generator - "Chundoong".... 96
Figure 5.3. Physical properties of HPM exposure system. (a) Diode voltage and diode... 102
Figure 5.4. Preliminary assessment of high power microwave-irradiated solutions for... 104
Figure 5.5. Evaluation of intracellular NO levels in U373MG cells treated with HPM-... 105
Figure 5.6. Evaluation of cell death after treatment with HPM-irradiated solutions. Cell... 107
Figure 5.7. Effect of HPM-irradiated solutions on the mitochondrial membrane and... 108
Figure 5.8. Effect of HPM-irradiated solution on transcription of cell death marker genes.... 109
Figure 6.1. Typical structure of coronaviruses. 115
Figure 6.2. Possible inactivation mechanisms of ozone against enveloped and non enveloped viruses. 115
Figure 6.3. An illustration of DBD plasma device. (a) DBD plasma mount (b) side view of... 118
Figure 6.4. Horizintal flowchart illustrating experimental procedure 119
Figure 6.5. Physical properties of DBD plasma and ozone measurement (a) Current-Voltage... 122
Figure 6.6. Mechanism for formation of ozone 122
Figure 6.7. Graphs indicating (a) % humidity levels at indicated PGO concentrations, (b)... 123
Figure 6.8. HCoV-229E infection and virus titer after PGO exposure. (a) HCoV-229E... 124
Figure 6.9. Effect of PGO on virus titer (a) Graphs showing %CPE at indicated PGO... 125
Figure 6.10. Evaluation of SI for PGO treatment (a) Graph showing cellular viability... 126
Figure 6.11. Effect of PGO on viral N gene expression and spike glycoprotein (a)... 127
Figure 6.12. Gene expression of antiviral host response genes (a) IRF1, (b) IRF2, (c) BIRC3,... 128
Figure 6.13. Illustration of possible mechanism for antiviral action of PGO against... 132
In recent decade, nonthermal plasma medicine has emerged as an innovative research domain combining plasma physics, chemistry, life science, and clinical medicine. Nonthermal plasma can be generated by addition of energy (heat or electromagnetic fields) to a neutral gas to make it electrically conductive. Plasma comprises of physical components such visible light and electromagnetic radiation, and chemical components such as free electrons, reactive oxygen/nitrogen species (ROS/RNS), free radicals, positively and negatively charged ions and excited gas molecules. Although the mechanisms for the nonthermal plasma effects are not fully understood, there is a consensus that cocktail of both physical components as well as chemical components play significant role in the mode of action. However, largescale research is required to improve and optimize for safe use in medical applications and extend the spectrum of clinical nonthermal applications. In this research, we elucidated the possible effects of periodic exposure of nonthermal plasma on skin cells, its impact on the crosstalk between skin fibroblasts and keratinocyte cells and cancer cells inhibition. Moreover, this study also revealed the anti-viral action of plasma generated ozone against coronavirus 229E strain.
First and foremost, we investigated the effect of nonthermal plasma on normal skin cell physiology. It is assumed that non-malignant cells are better to cope with elevated RONS levels. However, the effect of periodic stress on cellular homeostasis has not been thoroughly investigated in the plasma medicine field. So, the first study was aimed to determine the intrinsic alterations inside fibroblast cells after periodic plasma exposure in vitro. We observed changes in viability, cellular energetics, and cell cycle system under periodic redox stress conditions at weeks 3, 6, 9, and 12. Results indicate consistent increase in apoptosis, with accumulation of RONS and cell cycle arrest at the final stages. These results can provide an insight into the fibroblasts adaptation mechanism against several skin pathophysiologic conditions associated with oxidative stress conditions.
The next experiments were focused to investigate interactions that occur within skin cells at the onset of skin repair process. Keratinocytes and fibroblasts act as key players and interact extensively with each other during the skin repair. In this study, we observed the impact of non-thermal plasma generated oxidative stress on interactions between keratinocytes and fibroblasts. To this end, monoculture and coculture experimental setup of fibroblasts and keratinocytes was used. First, we observed the impact of plasma generated oxidative stress on the viability and energetics of both fibroblasts and keratinocytes. Further, results indicated that low doses exposure of plasma enhanced their proliferation rate, with upregulated expression of genes (KGF, MMP2, GMCSF, IL-6, and IL-8) in fibroblasts, indicating the activation of fibroblasts and onset of the repair process. Moreover, we observed enhanced migration under co-culture conditions under the given redox stress conditions indicating enhanced interactions between keratinocytes and fibroblasts. This observation was further reinforced by elevated expression of the upstream regulator and the effectors of the Hippo pathway (YAP and CYR61, respectively), which are associated with enhanced migration. Overall, this study demonstrates and reinforces use of nonthermal plasma in skin repair and wound physiology.
Next two studies were focused on cancer cell inhibition. Nonthermal plasma has been shown to inhibit various types of cancer with high selectivity and thus expected to be used extensively in cancer therapy for clinical application. Cancer cells generate high amount of ROS and can survive due to differently regulated transcriptome compared to non-cancerous cells. MicroRNAs (miRNA) are short non-coding RNAs which regulate approximately 30% of transcriptome. In this study, we investigated the plasma induced miRNAs in cancer cells. Over 2500 miRNAs were screened using next generation RNA sequencing. Approximately 1000 miRNAs were differentially expressed in melanoma (SK-2) cells after plasma treatment. Plasma induced miRNAs were shown to regulate cellular growth. Overall, this study helped to identify the key miRNAs involved in cellular ROS regulation after plasma treatment.
Next study was focused on the physical component of nonthermal plasma, particularly electromagnetic energy for cancer cell inhibition. Electromagnetic radiation (EM) is increasingly being used for several biological applications. Electromagnetic fields are capable of generating plasma or equivalent energy conditions. In this study, we focused to investigate the nonthermal effect of 3.5 GHz pulsed electromagnetic field-irradiated liquid solutions on growth of human malignant cells and nonmalignant cells. Phosphate buffered saline (PBS), deionized water, and Dulbecco's modified Eagle medium (DMEM) liquid solutions were irradiated with pulsed microwave radiation (45 shots with the energy of 1 mJ/shot). Results indicated that MW irradiation with power density ~ 12 kW/cm2 and electric field ~ 11 kV/cm could induce reactive nitrogen oxygen species in deionized water. We then evaluated cellular viability, energetics, mitochondrial membrane function, cell cycle phases, and cell death in cells. We observed alterations in the cell cycle, mitochondrial membrane potential, and cell death rates in malignant U373MG cells in MW irradiated water alone. Interestingly, this observation was limited to water and not in PBS or culture medium. Further, MW irradiated water induced changes in the expression of genes responsible for cell death. Overall, MW-irradiated water can change cellular physiology considerably, whereas irradiated culture media and PBS solutions could not induce significant changes which affect cellular health. This study highlights that physical components such as electromagnetic radiation may contribute with chemical components against cancer cell growth in the given conditions.
Finally, in the wake of COVID-19 pandemic, we investigated an important aspect of nonthermal plasma with respect to surface disinfection. A number of studies have been investigating current viral inactivation methods and finding novel options to contain the spread of virus. Nonthermal plasma has previously shown the ability to inactivate microbes and been used for biological decontamination and surface modifications. So, this study investigated the antiviral activity of plasma generated ozone against coronavirus 229E strain. Plasma ozone exposure for 4 h at 10 ppm ozone concentration was found to be sufficient to inactivate 99% virus infectivity. Further, it was also shown that plasma could reduce viral nucleocapsid mRNA expression and spike glycoprotein protein expression. Moreover, plasma induced mRNA expression of anti-viral machinery in host MRC-5 cells. Taken together, this study revealed the antiviral action of plasma against coronavirus 229E.
In conclusion, this study provides new insights of nonthermal application for skin physiology and cancer cell attenuation. Moreover, it also enlarges the spectrum of biological application including virus inactivation.*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
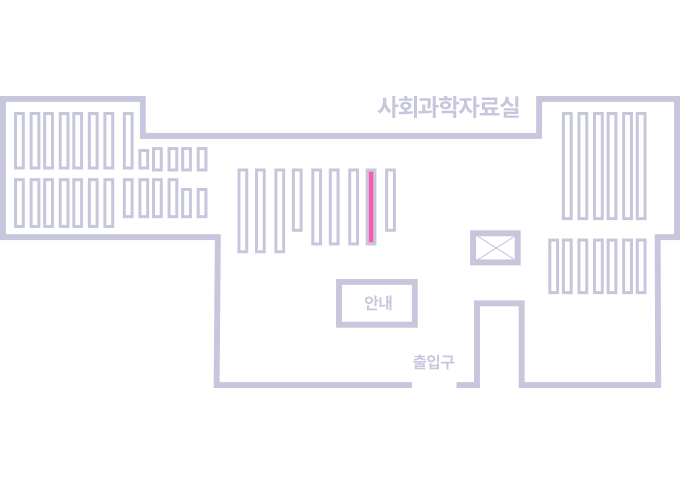
도서위치안내: / 서가번호:
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.