권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
Title Page
ABSTRACT
Contents
LIST OF ABBREVIATIONS 19
Chapter 1. Introduction 23
1.1. General background 24
1.2. Tailoring biomaterials for regulating macrophage fate: A literature review 29
1.2.1. Effect of biophysical properties on macrophage fate 29
1.2.2. Effect of biochemical properties on macrophage fate 32
1.2.3. Tissue-specific biomaterials for immunoengineering 35
1.2.5. 3D bioprinting and immunoengineering towards multi-modal tissue regeneration 36
1.2.6. Statement of Significance 40
1.3. Scope and Format of Dissertation 41
References 43
Chapter 2. 3D Bioprinting of Cellulose Nanocrystals-reinforced Alginate- Gelatin Bioinks for Accelerating Bone Regeneration 84
Abstract 84
2.1. Introduction 85
2.2. Experimental section 87
2.2.1. Materials 87
2.2.2. Bioink formulation 87
2.2.3. 3D printing 87
2.2.4. Bioink characterization 88
2.2.5. Evaluation of printing performance 88
2.2.6. In vitro studies 88
2.2.7. In vivo studies 91
2.2.8. Statistical analysis 91
2.3. Results and Discussion 92
2.3.1. Physico-chemical properties of the 3D printed scaffolds 92
2.3.2. Viscoelastic properties of the bioinks 93
2.3.3. Printability analysis of the developed bioinks 94
2.3.4. In vitro biocompatibility of the 3D printed scaffolds 95
2.4.5. 3D printed scaffolds promoted hBMSCs adhesion in vitro 96
2.3.6. 3D scaffolds enhanced the expression of osteoblastic gene markers 97
2.3.7. In vivo bone regeneration potential of the printed scaffolds 98
2.4. Summary 99
References 100
Chapter 3. 3D Bioprinting of Cellulose Nanoparticles-reinforced Bioinks with Enhanced Osteo-immunomodulatory Functions for Accelerating Bone Regeneration 120
Abstract 120
3.1. Introduction 121
3.2. Experimental section 122
3.2.1. Materials 122
3.2.2. Bioink preparation 122
3.2.3. 3D bioprinting 122
3.2.4. Characterization of the bioinks 123
3.2.5. Swelling and degradation study 123
3.2.7. Cell viability 124
3.2.8. Cell morphology 124
3.2.9. Alkaline phosphatase (ALP) activity and mineralization 125
3.2.10. RNA extraction and real-time polymerase chain reaction analysis 125
3.2.11. Immunocytochemical staining 126
3.2.12. Cytokine array 126
3.2.13. Macrophage polarization study 126
3.2.14. In vivo study 127
3.2.15. Statistical analysis 128
3.3. Results and Discussion 128
3.3.1. 3D-printing of the fabricated hydrogels 128
3.3.2. Spectroscopic analysis and recovery behavior 129
3.3.3. Swelling and degradation behavior of the scaffolds 131
3.3.4. Biocompatibility of the scaffolds 132
3.3.5. Osteogenic gene expression and pathway analysis 133
3.3.6. Macrophage polarization study 135
3.3.7. Macrophage mediated osteogenesis and migration study 137
3.3.8. In vivo bone regeneration potential and Histological analysis 137
3.4. Summary 138
References 140
Chapter 4. 3D Bioprinting of Conductive Gelatin/polypyrrole Bioinks with Direct Microcurrent Stimulation for Accelerating Bone Regeneration through Immunomodulation 160
Abstract 160
4.1. Introduction 161
4.2. Experimental Section 162
4.2.1. Materials 162
4.2.2. Synthesis and characterization of GelMA 162
4.2.3. Synthesis and characterization of PPy-grafted GelMA 163
4.2.4. Preparation of GelMA-PPy based conductive hydrogel 163
4.2.5. Characterization of GelMA-PPy hydrogel 163
4.2.6. 3D printing of conductive GelMA-PPy hydrogels 164
4.2.7. Electrochemical measurements 165
4.2.8. hBMSCs culture, 3D bioprinting, and in vitro osteogenic differentiation 165
4.2.9. Transcriptome analysis 166
4.3. Result and Discussion 166
4.3.1. Characterization of the GelMA-PPy ink 166
4.3.2. Conductivity, viscoelasticity, and printability of the GelMA-PPy ink 167
4.3.3. 3D printing of complex biological structures 171
4.3.4. Device setup and optimization of electric field for cell culture 172
4.3.5. In vitro bioactivity, 3D bioprinting, and osteogenic differentiation of stem cells 173
4.3.6. 3D culture model exhibited distinct transcriptomic profiles 175
4.3.7. 3D culture model sustains osteogenic capacity of hBMSCs via activating SMAD/NOTCH signaling pathways 177
4.4. Summary 177
References 179
Chapter 5. Light-assisted 3D Printing of Biomimetic Hydrogel Containing Carbon Dots@Nanocellulose for Image-guided Skin Regeneration 210
Abstract 210
5.1. Introduction 211
5.2. Experimental Section 212
5.2.1. Materials and reagents 212
5.2.2. 3D modeling and printer setup 213
5.2.3. Synthesis and characterization of CDs 213
5.2.4. Synthesis of CDs modified cellulose nanocrystals (T-CNC@CDs) 213
5.2.5. Electrochemical measurements 214
5.2.6. Synthesis of methacrylate grafted gelatin (GelMA) 214
5.2.7. Luminescent resin preparation and DLP printing 214
5.2.8. Characterization of the 3D printed hydrogels 215
5.2.9. Cell culture and biocompatibility 216
5.2.10. Statistical analysis 216
5.3. Results and Discussion 217
5.3.1. Characterization of the T-CNCs, N-CDs, and T-CNC@CDs 217
5.3.2. In vitro bioimaging property of T-CNC@CDs 218
5.3.3. Electrochemical properties of T-CNC@CDs 219
5.3.4. Structural, functional, and mechanical properties of the luminescent bio-resin 220
5.3.5. Study of photopolymerization kinetics and printability 223
5.3.6. 3D bioprinting of proof of concept model and image-guided tissue regeneration 225
5.4. Summary 226
References 228
Chapter 6. Immunopolarized Exosome-laden 3D Bioprinted Skin Grafts with All Functional Physiological Features for Skin Tissue Engineering 251
Abstract 251
6.1. Introduction 252
6.2. Experimental Section 254
6.2.1. Cell culture 254
6.2.2. Bioink fabrication 254
6.2.3. 3D Bioprinting 255
6.2.4. Characterizations 255
6.2.5. Macrophage phenotyping and RNA sequencing 256
6.2.6. Exosome isolation and characterization 257
6.2.7. Preparation of exosome-loaded d-ECM hydrogel and drug delivery study 258
6.2.8. Supporting bath-assisted 3D bioprinting of multi-layered skin construct 258
6.2.9. Histological evaluation of the bioprinted skin model 259
6.3.9. Statistical analysis 260
6.3. Results and Discussion 260
6.3.1. Characterization of the nanocomposite bioinks 260
6.3.2. Rheological investigation of the Group-I bioinks 261
6.3.3. 3D bioprinted AGP hydrogel promoted M2 macrophage polarization 262
6.3.4. M2 polarized exosome extraction and in vitro bioactivity evaluation 264
6.3.5. Extraction and characterization of chicken skin-derived d-ECM 265
6.3.6. Sustained delivery of Exos from d-ECM hydrogel promotes angiogenesis of hMSCs in vitro 266
6.3.7. 3D bioprinting of skin constructs with Exo-laden COL@d-ECM bioinks 267
6.4. Summary 270
Chapter 7. 3D Bioprinting of Polyphenolic Carbon Quantum Dots-reinforced Immunomodulatory Hydrogels for Multi-Modal Tissue Regeneration and Anti-Infection Therapy 281
Abstract 281
7.1. Introduction 282
7.2. Experimental section 284
7.2.1. Materials and instruments 284
7.2.2. Synthesis of the CQDs 284
7.2.3. Synthesis of methacrylated gelatin (GelMA) 285
7.2.4. Fabrication and characterization of the GelMA-CQDs bioinks 285
7.2.5. Photothermal properties of the fabricated hydrogels 285
7.2.6. 3D printing of the GelMA-CQD bioinks 286
7.2.7. In vitro studies 287
7.2.8. Drug loading and release study 291
7.2.9. NIR-triggered anti-osteosarcoma therapy 292
7.2.10. In vivo full-thickness skin regeneration study 292
7.2.11. In vivo bone regeneration study 292
7.2.12. Statistical analysis 293
7.3. Results and Discussion 293
7.3.1. Characterization of the polyphenolic CQDs 293
7.3.2. Antioxidant and anti-aging properties 296
7.3.3. Characterization and 3D printing of GelMA-CQDs bioinks 298
7.3.4. In vitro biocompatibility and wound healing study 301
7.3.5. In vivo wound healing in full-thickness wound model 302
7.3.6. Macrophage phenotyping and osteo-immunomodulation study 302
7.3.7. 3D printed GelMA-CQDs scaffold promoted in vitro angiogenic and osteogenic capabilities of hBMSCs 304
7.3.8. Immunomodulation-assisted enhanced osseointegration 305
7.3.9. In vitro drug delivery and NIR-triggered anti-osteosarcoma therapy 306
7.3.10. 3D printed GelMA-Y scaffold promotes vascularized bone regeneration in vivo 308
7.4. Summary 309
References 311
Chapter 8. Conclusions and Future Directions 334
ABSTRACT (KOREAN) 337
LIST OF PUBLICATIONS 340
LIST OF PATENTS 344
Figure 1.1. Mechanisms of macrophage activation and differentiation for tissue healing and regeneration. The macrophages secrete various chemokines and cytokines, which may regulate... 60
Figure 1.2. The various stages of the inflammatory response during the wound healing process. The pro-inflammatory phase of wound healing is mainly dominated by M1-like macrophages,... 61
Figure 1.3. Schematic illustration of the osteo-immunomodulation process. The macrophages are polarized through the yes-associated protein (YAP) signaling pathway under various stress... 62
Figure 1.4. Schematic illustration of the 3D bioprinting process. The first step of bioprinting starts with the medical imaging of tissues or organs (Step-I). The 3D image of the tissues and organs are... 63
Figure 1.5. Effect of biomaterial surface property (structure-function relationship) on immunomodulation of macrophages. The surface property of a biomaterial scaffold decides... 64
Figure 1.6. Effect of micro/nano PDMS patterning on macrophage polarization. (a & b) FE-SEM morphology of the Raw 264.7 cells growing on 2 µm PDMS pattern and flat PDMS surface... 65
Figure 1.7. Biophysical cues regulating the monocyte/macrophage fate. (a) Schematic illustration of the RGD-modified SPIONs regulating the macrophage polarization under varying frequency range. (b, c) FE-... 66
Figure 1.8. Schematic diagram of the working principle of (a) inkjet printing, (b) microextrusion printing, and (c) laser-assisted bioprinting. The inkjet printing utilizes thermal or piezoelectric... 67
Figure 1.9. (a) Examples of large-scale 3D bioprinted human organs with varying geometry. Researchers created cartilage, cardiac, kidney, skin, and aortic valve substitutes using various... 68
Figure 1.10. (a) Schematic diagram showing the blood vessel organization of an adult bone marrow. Bone marrow comprises numerous H-type blood vessels in the metaphysis region with osteoprogenitor cells. The... 69
Figure 1.11. Recent advances in 3D bioprinted osteo-immunomodulatory platforms for robust bone regeneration. (a & b) Glycopeptide-modified PCL/nHAp scaffold (1, 2) promoted robust bone regeneration... 70
Figure 2.1. Schematic illustration of 3D bioprinting of Alg/Gel/CNCs hydrogels for enhancing the proliferation and differentiation of human mesenchymal stem cells (hBMSCs). (a) Schematic... 104
Figure 2.2. CAD modeling and 3D printing setup. (a, b) Representative square (5 × 5 × 0.8 mm) and circular (5 × 5 × 0.8 mm) designs used for 3D printing in this study. (c) Digital photograph... 105
Figure 2.3. Morphology of the 3D printed hydrogel scaffolds. (a-r) Digital photographs of the Alg/Gel and its composite hydrogels before and after CaCl₂ crosslinking. (c-s) Digital... 106
Figure 2.4. The FT-IR spectra of the (a) pure polymers, and (b) its nanocomposites. The swelling efficiency of the developed hydrogel scaffolds (c) before and (d) after CaCl₂ crosslinking. 107
Figure 2.5. Viscoelastic property of the fabricated bioinks. (a, b) The frequency sweep (ω) test of the bioinks within 0.1 to 100 Rad s¯¹ range. Change in storage (G') and loss (G") modulus of the... 108
Figure 2.6. Assessment of printability of the developed bioinks. (a) Schematic illustration of the DIW-based 3D printing process. Inset is the digital photograph of the 3D printing of Alg/Gel... 109
Figure 2.7. Demonstration of 3D printing of big constructs using 4% CNC/Alg/Gel bioink. (a-d) Digital photographs of a 25 × 25 × 3 mm construct (infill density: 20%) with correspond ding... 110
Figure 2.8. In vitro biocompatibility assessment of the 3D printed hydrogels. (a) Schematic diagram of the cell culture. (b) Fluorescence (FL) microscopy images of hBMSCs showing the... 111
Figure 2.9. Evaluation of cytoskeletal protein markers expression of hBMSCs in the presence of 1% CNC/Alg/Gel. (a) FL images of DAPI-positive hBMSCs infiltrating into the 3D printed... 112
Figure 2.10. Evaluation of osteoblastic gene markers expression of hBMSCs in the 3D printed hydrogel scaffolds. (a-g) qRT-PCR analysis of hBMSCs in the presence of 1% CNC/Alg/Gel... 113
Figure 2.11. Evaluation of in vivo bone regeneration potential of the 3D printed scaffolds. (a) Digital photographs of the in vivo surgical procedure. (b) Representative uCT in vivo images of... 114
Figure 3.1. Schematic presentation for the fabrication of chitosan/silk fibroin/cellulose nanoparticles (CS/SF/CNPs) hydrogel, (a) The chemical structure of the used components, (b)... 144
Figure 3.2. (a) Schematic presentation for the designing of 3D construct from CAD program, (b) Photographs of the printed scaffolds, (c) Light microscopic images of the printed scaffolds, (d)... 145
Figure 3.3. Spectroscopic characterizations of the scaffolds, (a) FTIR spectra, (b) XRD patterns of the indicated scaffolds, (c) The storage modulus (G', solid lines) and loss modulus (G", without... 146
Figure 3.4. (a) Determination of the swelling potential of the fabricated scaffolds in the water at room temperature, (b) The degradation rate of the developed scaffolds in the PBS media, and (c)... 147
Figure 3.5. Cytotoxicity evaluation of the printed scaffolds in the presence of hBMSCs at different time periods, (a) Cell viability of hBMSCs in the presence of developed scaffolds at indicated time... 148
Figure 3.6. Evaluation of osteogenic differentiation potential of the fabricated scaffolds, (a) The relative expression of mRNA in hBMSCs with CS/SF/CNPs scaffolds and control after 7 and 14... 149
Figure 3.7. (a-d) Evaluation of the macrophage polarization potential of the printed scaffolds with Raw 264.7 cells by the FACS technique after 1 and 3 days of treatment, and (e) The... 150
Figure 3.8. (a) Evaluation of the osteo-immunomodulatory potential of the printed scaffolds with hBMSCs in the presence of macrophages-derived conditioned media (M-CM) (arrows indicate the... 151
Figure 3.9. In vivo study for the evaluation of the osteogenic potential of the printed scaffold, (a) The obtained CT images in different conditions. The circle shows the defective area in the rats.... 152
Figure 4.1. (a) Schematic illustration for the fabrication process of 3D printed triple-crosslinked (thermo-photo-ionic crosslinking) GelMA-PPy based hydrogel for improving the conductivity and... 183
Figure 4.2. (a) FE-SEM images of the freeze-dried (i) GelMA, (ii) GelMA-PPy, and (iii) GelMA- PPy-Fe crosslinked scaffolds. Insets are optical micrographs of the corresponding hydrogels.... 184
Figure 4.3. Rheological measurements of the formulated bioink. (a) Representative storage (G') and loss modulus (G") of the GelMA and GelMA-PPy bioink. The frequency sweep test was... 185
Figure 4.4. Evaluation of printability of the GelMA-PPy bioink. (a) Schematic illustration of the ink deposition process. (b) Schematic representation of the 3D printing of GelMA-PPy bioink with... 186
Figure 4.5. 3D printing of complex architectures showing the mechanical integrity using GelMA- PPy bioink. Demonstration of (a) square structure, (b) hollow cylinder, (c) hexagonal infill, and... 187
Figure 4.6. (a) Schematic illustration of the cell culture procedure showing the (i) surface cell seeding technique, and (ii) cell-laden culture technique, respectively. (b) WST-8 viability assay... 188
Figure 4.7. Macrophage polarization and Osseointegration potential of the fabricated scaffolds. (a) Schematic illustration of the experiment. (b) Flow cytometry analysis of the Raw 264.7 cells... 189
Figure 4.8. Transcriptomic analysis of hBMSCs-laden GelMA-PPy-Fe gels for osteogenesis. (a) A schematic workflow for 3D printing, cell culture, RNA isolation, and transcriptomic analysis... 190
Figure 4.9. Transcriptomic analysis for osteoblast differentiation of hBMSCs upon electrical stimulation. (a) K-means clustering heatmap of the DEGs in various groups showing the major... 191
Figure 4.10. Effect of electrical stimulation on cellular metabolism of hBMSCs. (a) Representative K-means clustering heatmap showing the DEGs associated with calcium hemostasis. (b) K-means... 192
Figure 4.11. Gene set enrichment analysis (GSEA) and gene ontology (GO) analysis of the 2D (positive control) vs. 3D (experimental) culture of hBMSCs under EFs stimulation. (a)... 193
Figure 5.1. Morphological and structural feature of the T-CNCs and N-CDs. (a) HR-TEM images of the T-CNCs. (b) HR-TEM images of the N-CDs showing the unique spherical morphology. (c)... 233
Figure 5.2. Preparation and characterization of the CNC-CDs nanocomposites. (a, b) Schematic illustration of the N-CDs synthesis and functionalization of T-CNCs via amide coupling. (c) Digital... 234
Figure 5.3. Electrochemical properties of the T-CNCs and CNC-CDs. (a) Cyclic voltammetry diagram (current vs. potential) of T-CNCs and CNC-CDs in the presence of 1× phosphate buffer... 235
Figure 5.4. Fabrication and characterization of the CNC-CDs based bio-resin for DLP printing. (a) Schematic illustration of the polymer library used for bio-resin preparation. (b) Schematic... 236
Figure 5.5. Morphological and structural features of the fabricated hydrogel scaffolds. (a) FE- SEM morphology with corresponding vertical and horizontal line-scan profiles of the freeze-dried... 237
Figure 5.6. Photopolymerization kinetics and performance of the developed bio-resins. (a) curing depth (Cd) of the GM, GPD, and GPCD bio-resins against UV irradiation dose (E) at 365 nm. (b)...[이미지참조] 238
Figure 5.7. 3D printing of GPCD bio-resin. (a) Schematic illustration of the resin preparation, CAD modeling, and 3D printing process using the GPCD bio-resin. (b) CAD model of the target... 239
Figure 5.8. DLP printing of model structures and assessment of in vitro biocompatibility using GPCD bio-resin. (a) The CAD model of the target constructs used in this study. (b) Digital... 240
Figure 5.9. 3D bioprinting of 'proof-of-concept' models using GPCD bio-resin. (a) Schematic illustration of the bioprinting process. The cells were mixed with the GPCD bio-resin and loaded onto the resin vat... 241
Figure 6.1. Characterization and bioactivity evaluation of the polydopamine nanospheres (PDA NSPs) and its composite hydrogel scaffolds. (a) HR-SEM image of the as-synthesized PDA NSPs.... 272
Figure 6.2. Viscoelastic property of the fabricated Group-I bioinks. (a) Representative storage modulus (G') modulus of the pure AG and its composite bioinks. (b) The loss (G") modulus of the... 273
Figure 6.3. Transcriptomic and morphological analysis of 3DP scaffold-assisted macrophage polarization. (a) Schematic diagram showing the phenotypic plasticity and exosome production in the... 274
Figure 6.4. Extraction and characterization of immunopolarized exosomes from Raw 264.7 cells. (a) Schematic illustration of the exosome induction and isolation used in this study. (b) Nano... 275
Figure 6.5. Extraction and characterization of the decellularized extracellular matrix (d-ECM). (a) Schematic diagram showing the overall extraction procedure of chicken skin d-ECM. (b)... 276
Figure 6.6. Evaluation of the exosome quality and in vitro angiogenic potential. (a) Schematic illustration of the exosome labelling with Dil (i) and fabrication of the exosome-laden bioink (ii).... 277
Figure 6.7. Supporting bath-assisted 3D bioprinting of the immunopolarized exosome-laden skin constructs. (a) Schematic illustration of the supporting bath-assisted skin bioprinting procedure.... 278
Figure 6.8. In vitro skin bioprinting with or without immunopolarized exosomes (mExo-AGP) and cytocompatibility evaluation. (a) Schematic illustration of the 3D bioprinting and cell culture... 279
Figure 7.1. Schematic illustration of the proposed mechanism of tissue repair and regeneration by the polyphenolic CQDs-incorporated hybrid scaffold. 317
Figure 7.2. Characterization of the polyphenolic CQDs. (a) Schematic diagram of the dual- emissive CQDs from phloroglucinol. (b, c) HR-TEM images of the as-prepared G-CQDs and Y-... 318
Figure 7.3. Evaluation of anti-aging and anti-oxidant properties of the dual-emissive CQDs. (a) DPPH radical scavenging assay of the CQDs with various formulations. Ascorbic acid and 1,3,5-... 319
Figure 7.4. Physico-chemical characterization of the hydrogel scaffold. (a) Digital photograph of the GelMA-G and GelMA-Y hydrogels under visible (day light) and UV light (365 nm). (b)... 320
Figure 7.5. Optimization of the GelMA-CQDs bioinks. (a) Schematic diagram of the bioink formulation and optimization strategy. (b) The shear moduli (G' and G") of the fabricated GelMA,... 321
Figure 7.6. In vitro biocompatibility test of the 3D printed hydrogel scaffolds. (a) The DPPH and enzyme inhibition assay of the pure GelMA and its composite scaffolds. (b) WST-8 assay of the... 322
Figure 7.7. Evaluation of in vivo skin regeneration ability of the 3D printed GelMA-CQDs scaffolds. (a) Schematic diagram for the experimental design. (b) Demonstration of the wound... 323
Figure 7.8. GelMA-CQDs scaffold enhanced macrophage viability and promoted M2 polarization in vitro. (a) Schematic diagram for the M2 polarization and osteo-immunomodulation. (b) FL microscopy images... 324
Figure 7.9. In vitro angiogenic and osteogenic potential of hBMSCs. (a) Representative bright field and FL images of hBMSCs showing the angiogenic sprouts in the presence of bioprinted... 325
Figure 7.10. Evaluation of osteo-immunomodulatory effects of macrophage-conditioned media (M-CM) on hBMSCs. (a, c) Representative ARS stained plates with optical micrographs of the 2D... 326
Figure 7.11. In vitro anti-osteosarcoma effect of the engineered GelMA-Y scaffold. (a) Schematic diagram of the NIR-responsiveness of the fabricated scaffolds. (b) Temperature profile as a function of time upon... 327
Figure 7.12. In vivo bone regeneration potential of the 3D printed scaffolds. (a) Digital photographs of the surgical procedure in rats and scaffold implantation. The yellow dotted circle... 328
Figure S2.1. In vitro biocompatibility evaluation of the developed hydrogel scaffolds. (a) Digital photographs of the printed constructs used for cytotoxicity evaluation. (b) WST-1 assay of hBMSCs... 117
Figure S2.2. In vitro bioactivity of the developed hydrogel scaffolds. (a, b) Wettability test of the 3D printed scaffolds using manual drop testing and contact angle measurement. (c) Quantification... 118
Figure S2.3. Representative bright field images of hBMSCs invading the scaffolds after (a-c) 3 days, and (d, e) 7 days of incubation. Scale bar: 100 µm. 119
Figure S3.1. (a) FT-IR spectra of the pure cellulose and cellulose nanoparticles (CNPs). (b, c) Representative 2D (2 μm x 2 μm) and 3D AFM morphology of the as-synthesized CNPs. 153
Figure S3.2. (a) Digital photograph of the filament formation test of the fabricated bioink. (b) Digital photograph of the DIW-based 3D printing process. (c) Mechanical stability of the 3D... 154
Figure S3.3. Calculation of the uniformity factor (U) of the fabricated bioinks. 155
Figure S3.4. FE-SEM morphology of the 3D printed scaffolds showing the surface morphology. Scale bar: 1 mm. 155
Figure S3.5. Representative Live/Dead assay of the hBMSCs in the presence of 3D printed scaffolds after 3 days of culture. The blue and red arrow indicates the presence of live and dead... 156
Figure S3.6. Immunohistochemical (IHC) analysis of the hBMSCs. (a) Representative optical micrographs showing the expression of Runx2, ALP, and OPN protein markers in the presence of... 156
Figure S3.7. Representative cytokine and MAPK signaling pathway-related antibody array results with corresponding quantification data. Data reported are mean ± s.d. of duplicate (n=2)... 157
Figure S3.8. WST-8 assay of the Raw 264.7 cells in the presence of 3D printed scaffolds at indicated time points. Data reported as mean ± s.d., statistical significance at *p<0.05 and **p<... 157
Figure S3.9. Flow cytometry analysis for the iNOS (Pro-inflammatory), CD68 (pro-inflammatory) and CD163 (anti-inflammatory) marker in Raw 264.7 cells in the presence of fabricated scaffolds... 158
Figure S4.1. (a) Physical appearance of the GelMA and GelMA-PPy foam. (b) FT-IR spectra of the Gelatin, GelMA, and GelMA-PPy foam. 194
Figure S4.2. ¹H-NMR spectra of the (a) GelMA and (b) GelMA-PPy. 195
Figure S4.3. (a) The viscosity vs. shear rate curve indicating the shear-thinning nature of the GelMA (15 wt.%) and GelMA-PPy-Fe (15 wt.%) bioink. (b) Yield stress (τ₀) of the GelMA and... 196
Figure S4.4. The injectability property of the fabricated GelMA-PPy-Fe (15 wt.%) hydrogel ink. (a) Digital photographs of the various needles used for injectability experiment. (b) Photographs... 197
Figure S4.5. Mechanical properties of the 3D printed GelMA-PPy-Fe (15 wt.%) hydrogel scaffolds after 7 days of incubation in PBS at 37 ℃. The mechanical stability was measured by... 198
Figure S4.6. Wettability measurement of the 3D printed hydrogel scaffolds. (a) Contact angle (°) measurement of the freeze-dried GelMA and GelMA-PPy-Fe scaffolds at 25 ℃. (b) Surface energy... 198
Figure S4.7. Evaluation of 3D printing of the pure GelMA (15 wt.%) bioink. (a) Digital photographs of the 3D printing of various architectures (Square, hexagonal, and hollow cylinder)... 199
Figure S4.8. Evaluation of printability of the GelMA-PPy-Fe bioink. (a) Calculation of the critical layer height as a function of printing speed. (b) Digital photographs of the 3D printed hollow... 200
Figure S4.9. Stability of the 3D printed GelMA and GelMA-PPy-Fe hydrogel scaffolds in PBS after 14 days of incubation at 37 ℃, during incubation (left) and after incubation (right). 200
Figure S4.10. Mechanical and conductive properties of the freshly 3D printed GelMA-PPy-Fe hydrogels. (a) Compressive stress-strain curve of the 3D printed cylindrical hydrogels (n=3). (b)... 201
Figure S4.11. (a) Raw design file of the microcurrent stimulation device. (b) Digital photographs demonstrating the procedure of device setup (1), assembly (2), and electrical stimulation (3-4).... 202
Figure S4.12. In vitro mineral induction property of the GelMA and GelMA-PPy-Fe hydrogel scaffolds w/o electrical stimulation (EFs). Representative ARS staining images showing the... 202
Figure S4.13. Comparison of the in vitro osteogenic differentiation in the presence of 2D (surface seeding) vs. 3D (cell encapsulated or 3D bioprinted) culture system in the presence of 250 mV/20... 203
Figure S4.14. Evaluation of the osteogenic gene and protein markers expression in various culture systems. (a-b) Heat map diagram of the qRT-PCR analysis showing the expression of major... 204
Figure S4.15. (a) The mapping rates (%) of the RNA-Seq data with the human genome. (b) Heat map showing the two-way hierarchical clustering based on DEGs between Control, 2D, and 3D... 205
Figure S4.16. Representative epigenetic markers that were either up- or down-regulated during 3D culture of hBMSCs associated with (a) Lysine demethylase, (b) Histone deacetylase, and (c)... 206
Figure S4.17. (a, b) Normalized gene expression of NOTCH and SMAD pathway-related markers during EFs stimulation of hBMSCs. (c, d) STRING interaction and enrichment network of the... 207
Figure S5.1. AFM images of the T-CNCs. (a) 2D image, and (b) 3D surface plot. Scale bar: 2 µm. 243
Figure S5.2. FT-IR spectra of the pure T-CNCs, N-CDs, and CNC-CDs. 244
Figure S5.3. 2D SAXS pattern of the T-CNCs and T-CNC@CDs aqueous solution. The mass of the T-CNCs and T-CNC@CDs were taken 0.8 wt.% to compare the dispersion test. Scale bar... 244
Figure S5.4. (a) Current vs. potential curve of (a) T-CNCs and (b) showing the current stability within five oxidation-reduction cycles. Insets are the magnified graphs showing anodic current... 244
Figure S5.5. ¹H-NMR spectra of (a) pure gelatin, and (b) freeze-dried GelMA in D₂O. 245
Figure S5.6. Representative shear moduli (storage modulus/G' and loss modulus/G") of the fabricated bio-resins (a) before, and (b) after UV crosslinking. 246
Figure S5.7. The Power-law fitting (Ostwald model) of viscosity vs. varying shear rate of the GM, GPD, and GPCD bio-resins showing the shear-thinning property. 246
Figure S5.8. (a) Schematic representation of the photo-rheology setup. The polymer solution was injected into the platform and the viscosity (1 s¯¹ shear rate) was measured w/o or w/ UV... 247
Figure S5.9. Swelling efficiency of the 3D printed hydrogel scaffolds after 24 h of soaking in PBS at 37 ℃. Data are mean ± s.d. of triplicated experiments (n=3), statistical significance at *p<0.05. 247
Figure S5.10. The FT-IR spectra of the developed hydrogel (GM, GPD, and GPCD) scaffolds. 248
Figure S5.11. Digital photographs of the 3D printed GPCD hydrogels with (a) Square lattice, and (b) hexagonal lattice with varying infill and lattice densities. Scale bar: 5 mm. 248
Figure S5.12. Cell viability of hDFs in the presence of 3D printed hydrogels using WST-8 assay. Data are mean ± s.d. of triplicate (n=3) experiments, statistical significance at *p<0.05 and **p<0.01. 249
Figure S5.13. Representative Live/Dead assay of the Raw 264.7 cells in the presence of 3D printed hydrogels (GM, GPD, and GPCD) after 24 h of culture. Scale bar: 0.3 mm. 249
Figure S5.14. Cell viability of hBMSCs in the presence of 3D printed hydrogels using WST-8 assay. Data are mean ± s.d. of triplicate (n=3) experiments, statistical significance at *p<0.05. 250
Figure S7.1. Digital photographs of the precursor (1,3,5-trihydroxybenzene), G-CQDs, and Y- CQDs. 330
Figure S7.2. (a-c) ¹H-NMR spectra of the pure 1, 3, 5-trihydroxybenzene, G-CQDs, and Y-CQDs. (d-f) ¹³C-NMR spectra of the pure 1, 3, 5-trihydroxybenzene, G-CQDs, and Y-CQDs. 330
Figure S7.3. (a) XRD spectra of the pure 1, 3, 5-trihydroxybenzene, G-CQDs, and Y-CQDs. (b) FT-IR spectra of the pure 1, 3, 5-trihydroxybenzene, G-CQDs, and Y-CQDs. 331
Figure S7.4. The zeta potential of the as-prepared G-CQDs and Y-CQDs in DI water. 331
Figure S7.5. Quantitative data of the hDFs migration in the presence of scaffold leaching media after 24 h of incubation. Data are reported as mean ± s.d. (n=3), *p<0.05. 331
Figure S7.6. Graphical illustration of the M-CM perpetration and osteo-immunomodulation study of hBMSCs. 332
Scheme 5.1. Schematic illustration of the nanocellulose-based luminescent bio-resin preparation and key features for image-assisted tissue regeneration study. 232
Scheme 6.1. Schematic illustration of the bioink development for anti-inflammatory exosomes production and skin bioprinting towards skin regeneration. 271
본 논문에서는 단핵구/대식세포의 운명을 항염증 표현형으로 조작하기 위해 다양한 토폴로지, 화학적 조성 및 생체 활성 모이어티(나노필러)를 사용하여 3D 생체 인쇄 면역조절 소프트 스캐폴드를 제작하였다. 각 챕터에서 제작된 3D 스캐폴드는 뛰어난 생체 활성을 보였고 뼈와 피부 조직 재생을 위해 M2 표현형 단핵구/대식세포 분극화를 강화하였다. 또한, 뛰어난 기계적 특성을 가진 다양한 나노복합체 바이오잉크의 3D 바이오프린팅을 성공적으로 인쇄하였다. 셀룰로오스 나노결정과 셀룰로오스 나노입자 첨가로 제조된 바이오잉크 맞춤형 표면 특성은 팽윤 효율을 향상시켰을 뿐만 아니라 우수한 전단담화 (shear thinning) 및 전단농화(shear thickening)특성을 나타내어 3D 바이오프린팅에 이상적으로 출력되었다. 알지네이트와 젤라틴의 첨가는 배양된 중간엽줄기세포 (hBMSCs)에 더 큰 접착력, 산소 투과성 및 영양분 교환을 선호하는 동적 반내부 침투 폴리머 네트워크(semi-IPN)를 제공하였다. 키토산 매트릭스에 피부 피브로인을 첨가하면 다양한 표면(CD163) 및 세포학적(iNOS 또는 NOS2) 마커를 발현하여 인쇄 가능성이 향상되고 대식세포 부착 및 M2 분극화가 촉진하였다. 바이오프린팅된 다당류/단백질 하이드로겔 또한 염증 없이 강력한 생체 내 조직 재생 능력을 보여주었다.
중간엽 줄기세포 증분화 및 촉진을 위해 폴리피롤/젤라틴 메타크릴로일을 사용하는 금속 촉매 전기 전도성 하이드로겔 플랫폼을 제작하였고, 전기 자극 시 골 형성 동안 더 높은 증식, 분화 및 전사체 변화를 나타내었다. 또한, M2-분극 대식세포의 세포외 소포(엑소좀)가 d-ECM 기반 바이오프린팅 구조물에서 혈관신생 및 섬유아세포 증식을 개선함으로써 피부재생을 가속화한다는 것을 보여주었다. 따라서, 강화된 항골육종 요법으로 내인성(뼈) 및 외인성(피부) 조직 재생을 가속할 수 있도록 폴리페놀성 CQD/젤라틴 메타크릴로일을 사용하여 새로운 '다기능' 3D 생체 인쇄 면역 조절 플랫폼의 제조 또한 보고하였다. 각 논문 실험은 최소 세 번 수행되었으며 데이터는 광범위한 문헌 검토에 비추어 적절한 정당성과 함께 제시되었다. 본 논문에 제시된 데이터는 재현성과 신뢰성이 높아 임상적으로 적절한 임플란트를 만드는 데 도움이 될 수 있을것으로 사료된다. 본 연구결과는 인쇄 가능성, 생분해성, 생체 적합성 및 면역 유발 특성에 대한 정밀한 제어가 부족한 3D 바이오프린팅의 기존 장벽을 능가하는 데 도움이 될것으로 사료된다.이미 보고된 선행연구에 따르면 기존의 3D 프린팅 하이드로겔은 2D 배양에 적합하고 실제 생체 내 미세 환경이 부족한 스캐폴드 형태로만 사용할 수 있었다. 본 연구에서 시도된 바이오잉크는 기술 및 실험적 관점에서 맞춤형 표면 기능을 갖춘 하이드로겔 및 스캐폴드 형태 및 물리화학적 모두에서 안정적인 인쇄 가능한 바이오잉크 개발을 입증하였다. 제작된 바이오잉크는 바이오프린팅에 적합할 뿐만 아니라 조직 재생을 촉진하기 위한 약물 및 성장 인자와 같은 치료 분자의 전달에도 유리하였다. 마지막으로, 본 논문에서 제시된 결과는 생체 내 조직 치유 및 재생, 특히 환자별 치료 및 약물 스크리닝을 위한 차세대 이식형 플랫폼 개발에 도움이 될 것으로 사료된다.
이 논문에서 단핵구/대식세포에서 면역 조절을 촉진하기 위한 맞춤형 물리화학적 특성을 가진 6 가지 다른 바이오잉크 제작을 시연하였다. 바이오잉크는 뼈와 피부 재생을 위한 다양한 생체모방 모델을 구성하기 위해 직접잉크쓰기(DIW, Direct Ink Writing) 3D 프린팅 및 디지털광처리(DLP, Digital Light Processing) 기반 3D 프린팅에 활용되었다. 흥미롭게도, 바이오잉크는 다양한 수학적 모델을 통해 예측된 바와 같이 전단담화 및 주사 가능한 특성이 매우 높았다. 본 연구에서는 인간 골 중간엽 줄기 세포(hBMSCs), 인간 피부 세포(hDFs 및 hKCs), 쥐 대식세포 및 골격근세포(Raw 264.7 및 C2C12), 인간 골육종 세포(MG-63) 및 인간 내피 세포(hECs)를 사용하여 시험관 내 뼈 및 피부 유사체를 제작하였고, 결과로는 세포의 증식 및 분화 가능성이 스캐폴드 토폴로지, 표면 작용기, 생체 활성 성분(나노입자/성장인자/엑소좀), 하이드로겔의 다공성 및 생물물리학적 자극 존재에 의해 크게 영향을 받는다는 것을 입증하였다. 또한 3D 바이오프린팅된 스캐폴드는 각각 칼바리아 (calvaria critical) 결함 모델과 전체 두께 피부 손상 모델의 생체 내 시스템에서 우수한 생체조직재생을 유도하는 것으로 나타내었다.
앞에서 언급한바와 같이, 본 논문에서는 세포 캡슐화 및 3D 바이오 프린팅을 위한 일련의 생체 적합성 잉크를 개발하였으며, 바이오잉크 특성은 나노로드 또는 나노입자, 금속 이온, 단백질/펩티드의 도입, 표면 토폴로지(예: 다공성, 거칠기 또는 화학적 조성)와 같은 다양한 전략을 사용하여 단핵구/대식세포에서 특정 면역 조절 기능을 유도하였다. 뼈와 피부 조직 재생을 위해 논문 구성중 Part 1은 향상된 골 면역 조절 특성을 가진 새로운 바이오잉크 개발에 중점을 두었고 이를 바탕으로 인간 중간엽 줄기세의 증식, 분화 및 개선된 골유착 및 생체 내 뼈 재생을 위한 대식세포 보조 골 면역 조절에 미치는 영향을 조사하였다. Part II에서는 탄소 기반 물질과 탈세포화된 세포외 기질(d-ECM)에서 파생된 새로운 바이오잉크 제작을 통해 인간 진피 섬유아세포로부터 피부재생 증분화효과에 미치는 영향 및 면역 조절 반응을 분석하였다. 특히, 이미징 유도 조직 재생(비침습적 바이오프린팅)을 위한 초고휘도 형광 특성을 가진 바이오잉크 제작과 면역 분극화된 엑소좀/d-ECM/콜라겐으로 구성된 새로운 바이오잉크를 제작하여 피부조직 재생효과를 유도하였다. 마지막 Part III에서는 약물의 지속적인 전달을 통한 외인성(피부) 및 내인성(뼈) 조직 치유 및 항감염을 위한 차세대 '다기능' 바이오프린팅 플랫폼 개발에 중점을 두었으며 젤라틴 메타크릴레이트와 폴리페놀 탄소 양자점(CQD)으로 구성된 나노하이브리드 바이오잉크는 M2(상처치유와 항염) 대식세포 분극화와 강력한 조직재생이 향상되는 결과를 보였다. 또한, CQD으로 구성된 나노하이브리드 바이오잉크의 근적외선 조사시, 골육종 세포의 생리학적 미세 환경인 pH 6.5 에서 약물(독소루비신 및 파클리탁셀)의 지속 방출이 제어될 수 있음을 확인하였다. 그 결과, 본 연구에서 제작된 바이오잉크는 뼈 및 피부 세포와 생체적합성이 우수하고 생체 내 독성이 낮으며, 면역조절 효과가 뛰어남을 확인하였다. 본 연구논문에서는 바이오프린팅의 물리화학적 구조와 생물학적 기능 관계의 Cross-Talk 측면에서 보고하였으며, 향후 연구는 직접 뼈/피부 등의 바이오 프린팅을 위한 골 면역 조절, 물리적 신호 및 인쇄 가능성 최적화의 신호 경로에 대한 심층 연구에 주로 초점을 맞추고자 한다.*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
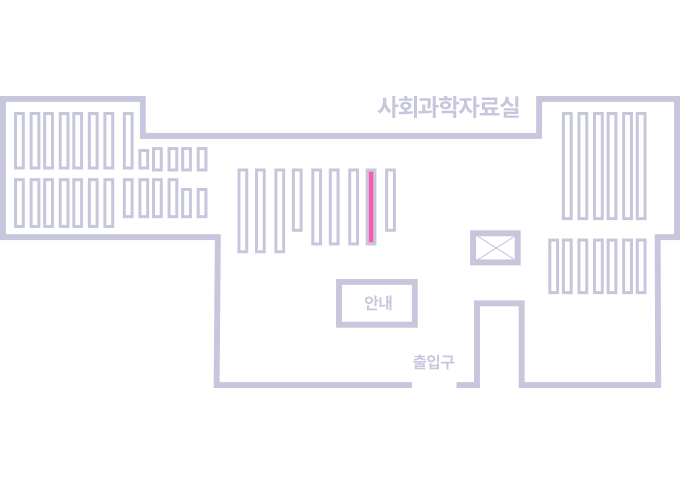
도서위치안내: / 서가번호:
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.