권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
Objective: This study aimed to analyze the prevalence and nutritional status of patients with dysphagia using the National Health Insurance Claim database collected from all Koreans.
Methods: According to the claim data from the National Health Insurance Service from 2007 to 2017, we calculated the prevalence, comorbidity, and direct medical costs of dysphagia patients. We analyzed the difference in medical costs according to the malnutrition rate and presence of malnutrition.
Results: The prevalence of dysphagia was 635.4 per 100,000 population in 2007 but increased to 1031.6 in 2017. The proportions of type insurance showed an increasing trend in both health insurance and national free medical care, while nursing hospitals showed a significant increase of 8.46%. Esophageal and gastrointestinal disorders accounted for the highest number of diseases with dysphagia. The average medical expense per person for dysphagia was11,984,632 Korea Won (KRW), and the average length of hospital stay was 154.1 days. The malnutrition rate of patients with dysphagia was 686.8 out of 100,000 people in 2007 to 362.9 out of 100,000 people in 2017. The malnourished group had 70.7 more inpatient hospital stays and nine more outpatient visits than the non-malnourished group.
Conclusion: The proportion of nursing hospitals and medical expenses increased significantly in the number of patientswith dysphagia, and the length of hospital stay and medical costs were higher with malnutrition. As incidence of dysphagia patients may increase due to aging, active management of dysphagia is required to improve the patient’s prognosis and quality of life.*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
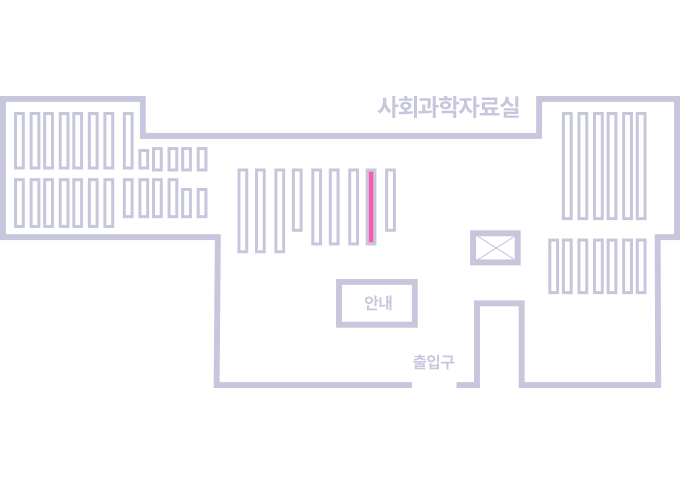
도서위치안내: 정기간행물실(524호) / 서가번호: 국내03
2021년 이전 정기간행물은 온라인 신청(원문 구축 자료는 원문 이용)
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.