권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
Background/Aims: Endoscopic visualization of the microscopic anatomy can facilitate the real-time diagnosis of pancreatobiliary disorders and provide guidance for treatment. This study aimed to review the technique, image classification, and diagnostic performance of confocal laser endomicroscopy (CLE).
Methods: We conducted a systematic review of CLE in pancreatic and biliary ducts of humans, and have provided a narrative of the technique, image classification, diagnostic performance, ongoing research, and limitations.
Results: Probe-based CLE differentiates malignant from benign biliary strictures (sensitivity, ≥89%; specificity, ≥61%). Needle-based CLE differentiates mucinous from non-mucinous pancreatic cysts (sensitivity, 59%; specificity, ≥94%) and identifies dysplasia. Pancreatitis may develop in 2-7% of pancreatic cyst cases. Needle-based CLE has potential applications in adenocarcinoma, neuroendocrine tumors, and pancreatitis (chronic or autoimmune). Costs, catheter lifespan, endoscopist training, and interobserver variability are challenges for routine utilization.
Conclusions: CLE reveals microscopic pancreatobiliary system anatomy with adequate specificity and sensitivity. Reducing costs and simplifying image interpretation will promote utilization by advanced endoscopists.| 기사명 | 저자명 | 페이지 | 원문 | 목차 |
|---|---|---|---|---|
| 2021 Korean society of gastrointestinal endoscopy clinical practice guidelines for endoscopic sedation | Hong Jun Park, Byung-Wook Kim, Jun Kyu Lee, Yehyun Park, Jin Myung Park, Jun Yong Bae, Seung Young Seo, Jae Min Lee, Jee Hyun Lee, Hyung Ku Chon ... [et al.] | p. 167-182 |
|
|
| Can computed tomography colonography replace optical colonoscopy in detecting colorectal lesions? : state of the art | Alessia Chini, Michele Manigrasso, Grazia Cantore, Rosa Maione, Marco Milone, Francesco Maione, Giovanni Domenico De Palma | p. 183-190 |
|
|
| Single use (disposable) duodenoscope : recent development and future | Kihyun Ryu, Sunguk Jang | p. 191-196 |
|
|
| Confocal laser endomicroscopy in the diagnosis of biliary and pancreatic disorders : a systematic analysis | Do Han Kim, Somashekar G. Krishna, Emmanuel Coronel, Paul T. Kröner, Herbert C. Wolfsen, Michael B. Wallace, Juan E. Corral | p. 197-207 |
|
|
| (Commentary) A novel aerosol-exposure protection mask for patients during upper endoscopy | Soo-Jeong Cho | p. 208-209 |
|
|
| (Commentary) Fecal calprotectin as a surrogate marker for mucosal healing after initiating the therapeutic anti-tubercular trial | Satimai Aniwan | p. 210-212 |
|
|
| (Commentary) Predicting malignancy by peroral pancreatoscopy of an intraductal papillary mucinous neoplasm with a dilated main pancreatic duct : is seeing enough? | Yun Nah Lee, Jong Ho Moon | p. 213-214 |
|
|
| Perception of gastrointestinal endoscopy personnel on society recommendations on personal protective equipment, case selection, and scope cleaning during COVID-19 pandemic : an international survey study | Parit Mekaroonkamol, Kasenee Tiankanon, Rapat Pittayanon, Wiriyaporn Ridtitid, Fariha Shams, Ghias Un Nabi Tayyab, Julia Massaad, Saurabh Chawla, Stanley Khoo, Siriboon Attasaranya, Nonthalee Pausawasdi, Qiang Cai, Thawee Ratanachu-ek, Pradermchai Kongkham, Rungsun Rerknimitr | p. 215-225 |
|
|
| Preclinical efficacy and clinical feasibility of a novel aerosol-exposure protection mask for esophagogastroduodenoscopy | Mai Ego Makiguchi, Seiichiro Abe, Yutaka Okagawa, Satoru Nonaka, Haruhisa Suzuki, Shigetaka Yoshinaga, Ichiro Oda, Okamoto Ryuta, Yutaka Saito | p. 226-233 |
|
|
| Propofol alone versus propofol in combination with midazolam for sedative endoscopy in patients with paradoxical reactions to midazolam | Ji Hyung Nam, Dong Kee Jang, Jun Kyu Lee, Hyoun Woo Kang, Byung-Wook Kim, Byung Ik Jang | p. 234-239 |
|
|
| Risk stratification in cancer patients with acute upper gastrointestinal bleeding : comparison of glasgow-blatchford, rockall and AIMS65, and development of a new scoring system | Matheus Cavalcante Franco, Sunguk Jang, Bruno da Costa Martins, Tyler Stevens, Vipul Jairath, Rocio Lopez, John J. Vargo, Alan Barkun, Fauze Maluf-Filho | p. 240-247 |
|
|
| Efficacy and safety of endoscopic submucosal dissection for superficial gastric neoplasms : a Latin American cohort study | Fernando Palacios-Salas, Harold Benites-Goñi, Luis Marin-Calderón, Paulo Bardalez-Cruz, Jorge Vásquez-Quiroga, Edgar Alva-Alva, Bryan Medina-Morales, Jairo Asencios-Cusihuallpa | p. 248-255 |
|
|
| Value of fecal calprotectin measurement during the initial period of therapeutic anti-tubercular trial | Hyeong Ho Jo, Eun Young Kim, Jin Tae Jung, Joong Goo Kwon, Eun Soo Kim, Hyun Seok Lee, Yoo Jin Lee, Kyeong Ok Kim, Byung Ik Jang | p. 256-262 |
|
|
| Factors predicting difficult biliary cannulation during endoscopic retrograde cholangiopancreatography for common bile duct stones | Hirokazu Saito, Yoshihiro Kadono, Takashi Shono, Kentaro Kamikawa, Atsushi Urata, Jiro Nasu, Haruo Imamura, Ikuo Matsushita, Tatsuyuki Kakuma, Shuji Tada | p. 263-269 |
|
|
| Peroral pancreatoscopy with videoscopy and narrow-band imaging in intraductal papillary mucinous neoplasms with dilatation of the main pancreatic duct | Yui Kishimoto, Naoki Okano, Ken Ito, Kensuke Takuma, Seiichi Hara, Susumu Iwasaki, Kensuke Yoshimoto, Yuto Yamada, Koji Watanabe, Yusuke Kimura, Hiroki Nakagawa, Yoshinori Igarashi | p. 270-278 |
|
|
| Role of endoscopic ultrasound-guided fine-needle aspiration in the evaluation of abdominal lymphadenopathy of unknown etiology | Nonthalee Pausawasdi, Kotchakon Maipang, Tassanee Sriprayoon, Phunchai Charatcharoenwitthaya | p. 279-286 |
|
|
| Acute liver failure secondary to hepatic infiltration of malignant melanoma | Yujin Lee, Jaekwang Lee, Hyunsoo Kim, Changkeun Park, Jaekwon Jung, Daejin Kim, Yun Jin Chung, Hanjun Ryu | p. 287-291 |
|
|
| Endoscopic treatment of iatrogenic perforation of sigmoid diverticulum : a case report of multidisciplinary management | Giacomo Emanuele Maria Rizzo, Giuseppina Ferro, Giovanna Rizzo, Giovanni Di Carlo, Alessandro Cantone, Gaetano Giuseppe Di Vita, Carmelo Sciumè | p. 292-296 |
|
|
| Successful removal of a difficult common bile duct stone by percutaneous transcholecystic cholangioscopy | Hyunsuk Lee, Sang Hyub Lee, Gunn Huh, Yeji Kim, Saebeom Hur, Moonhaeng Hur, Minwoo Lee, Byeongyun Ahn | p. 297-301 |
|
|
| Endoscopic ultrasound-guided transgastric puncture and drainage of an adrenal abscess in an immunosuppressed patient | Carlos Andrés Regino, Jean Paul Gómez, Gabriel Mosquera-Klinger | p. 302-304 |
|
|
| Endoscopic ultrasonography findings for Brunner's gland hamartoma in the duodenum | Kyong Joo Lee, Bonil Park, Hee Man Kim | p. 305-309 |
|
|
| Large jejunal phytobezoar with small bowel obstruction treated by single-balloon enteroscopy | Eun Young Park, Dong Hoon Baek, Bong Eun Lee, Gwang Ha Kim, Geun Am Song | p. 310-312 |
|
|
| (A) rare cause of subepithelial tumor in the gastric fundus | Da Mi Kim, Gwang Ha Kim, Kyungbin Kim | p. 313-314 |
|
|
| (Letters To The Editor) Emergence of a new optical marker for colorectal neoplasms : to what extent should we accept it? | Han Hee Lee | p. 315-317 |
|
| 번호 | 참고문헌 | 국회도서관 소장유무 |
|---|---|---|
| 1 | Kochhar G, Wallace MB. Virtual histology in everyday gastrointestinal endoscopy. Clin Gastroenterol Hepatol 2018;16:1556-1561. | 미소장 |
| 2 | Trindade AJ, Leggett CL, Chang KJ. Volumetric laser endomicroscopy in the management of Barrett’s esophagus. Curr Opin Gastroenterol 2017;33:254-260. | 미소장 |
| 3 | Al-Mansour MR, Caycedo-Marulanda A, Davis BR, et al. SAGES TAVAC safety and efficacy analysis confocal laser endomicroscopy. Surg Endosc 2021;35:2091-2103. | 미소장 |
| 4 | Glover B, Teare J, Patel N. The status of advanced imaging techniques for optical biopsy of colonic polyps. Clin Transl Gastroenterol 2020;11:e00130. | 미소장 |
| 5 | RuffS, Curtin B, Quezado M, et al. Evaluation of confocal endoscopic microscopy for detection of early-stage gastric cancer in hereditary diffuse gastric cancer (HDGC) syndrome. J Gastrointest Oncol 2019;10:407-411. | 미소장 |
| 6 | Su P, Liu Y, Lin S, et al. Efficacy of confocal laser endomicroscopy for discriminating colorectal neoplasms from non-neoplasms: a systematic review and meta-analysis. Colorectal Dis 2013;15:e1-e12. | 미소장 |
| 7 | Yu X, Chen J, Zheng L, Song J, Lin R, Hou X. Quantitative diagnosis of atrophic gastritis by probe-based confocal laser endomicroscopy. Biomed Res Int 2020;2020:9847591. | 미소장 |
| 8 | Buchner AM. Confocal laser endomicroscopy in the evaluation of inflammatory bowel disease. Inflamm Bowel Dis 2019;25:1302-1312. | 미소장 |
| 9 | Zhang MM, Zhong N, Wang X, et al. Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy for diagnosis of gastric subepithelial tumors: a pilot study. Endoscopy 2019;51:560-565. | 미소장 |
| 10 | Pohl H, Tanczos BT, Rudolph B, et al. Probe-based confocal laser microscopy identifies criteria predictive of active celiac sprue. Dig Dis Sci 2012;57:451-457. | 미소장 |
| 11 | Cellvizio® Gastrointestinal Brochure - International [Internet]. Paris:Mauna Kea Technologies; c2016 [cited 2021 June 25]. Available from:https://www.maunakeatech.com/en/researchers/32-brochure. | 미소장 |
| 12 | Saadi M, Yu C, Othman MO. A review of the challenges associated with the diagnosis and therapy of primary sclerosing cholangitis. J Clin Transl Hepatol 2014;2:45-52. | 미소장 |
| 13 | Hutchins GF, Draganov PV. Cystic neoplasms of the pancreas: a diagnostic challenge. World J Gastroenterol 2009;15:48-54. | 미소장 |
| 14 | Gao YD, Qu YW, Liu HF. Comparison of diagnostic efficacy between CLE, tissue sampling, and CLE combined with tissue sampling for undetermined pancreaticobiliary strictures: a meta-analysis. Scand J Gastroenterol 2018;53:482-489. | 미소장 |
| 15 | Facciorusso A, Buccino VR, Sacco R. Needle-based confocal laser endomicroscopy in pancreatic cysts: a meta-analysis. Eur J Gastroenterol Hepatol 2020;32:1084-1090. | 미소장 |
| 16 | Njei B, McCarty TR, Varadarajulu S, Navaneethan U. Systematic review with meta-analysis: endoscopic retrograde cholangiopancreatography-based modalities for the diagnosis of cholangiocarcinoma in primary sclerosing cholangitis. Aliment Pharmacol Ther 2016;44:1139-1151. | 미소장 |
| 17 | Liu Y, Lu Y, Sun B, et al. Probe-based confocal laser endomicroscopy for the diagnosis of undetermined biliary stenoses: a meta-analysis. Clin Res Hepatol Gastroenterol 2016;40:666-673. | 미소장 |
| 18 | Fugazza A, Gaiani F, Carra MC, et al. Confocal laser endomicroscopy in gastrointestinal and pancreatobiliary diseases: a systematic review and meta-analysis. Biomed Res Int 2016;2016:4638683. | 미소장 |
| 19 | Konjeti VR, McCarty TR, Rustagi T. Needle-based confocal laser endomicroscopy (nCLE) for evaluation of pancreatic cystic lesions: a systematic review and meta-analysis. J Clin Gastroenterol 2022;56:72-80. | 미소장 |
| 20 | Peter S, Council L, Bang JY, et al. Poor agreement between endoscopists and gastrointestinal pathologists for the interpretation of probebased confocal laser endomicroscopy findings. World J Gastroenterol 2014;20:17993-18000. | 미소장 |
| 21 | Luthra AK, Pusateri AJ, Pfeil SA, et al. Confocal laser endomicroscopy interpretation and differentiation of pancreatic cysts: a randomized trial of teaching modalities. Techniques and Innovations in Gastrointestinal Endoscopy 2021;23:8-17. | 미소장 |
| 22 | Gerhards MF, Vos P, van Gulik TM, Rauws EA, Bosma A, Gouma DJ. Incidence of benign lesions in patients resected for suspicious hilar obstruction. Br J Surg 2001;88:48-51. | 미소장 |
| 23 | Shah RJ, Langer DA, Antillon MR, Chen YK. Cholangioscopy and cholangioscopic forceps biopsy in patients with indeterminate pancreaticobiliary pathology. Clin Gastroenterol Hepatol 2006;4:219-225. | 미소장 |
| 24 | Meining A, Chen YK, Pleskow D, et al. Direct visualization of indeterminate pancreaticobiliary strictures with probe-based confocal laser endomicroscopy: a multicenter experience. Gastrointest Endosc 2011;74:961-968. | 미소장 |
| 25 | Wallace M, Lauwers GY, Chen Y, et al. Miami classification for probebased confocal laser endomicroscopy. Endoscopy 2011;43:882-891. | 미소장 |
| 26 | Caillol F, Filoche B, Gaidhane M, Kahaleh M. Refined probe-based confocal laser endomicroscopy classification for biliary strictures: the Paris Classification. Dig Dis Sci 2013;58:1784-1789. | 미소장 |
| 27 | Wang KK, Carr-Locke DL, Singh SK, et al. Use of probe-based confocal laser endomicroscopy (pCLE) in gastrointestinal applications. A consensus report based on clinical evidence. United European Gastroenterol J 2015;3:230-254. | 미소장 |
| 28 | ASGE Standards of Practice Committee, Chathadi KV, Chandrasekhara V, et al. The role of ERCP in benign diseases of the biliary tract. Gastrointest Endosc 2015;81:795-803. | 미소장 |
| 29 | Tringali A, Lemmers A, Meves V, et al. Intraductal biliopancreatic imaging:european society of gastrointestinal endoscopy (ESGE) technology review. Endoscopy 2015;47:739-753. | 미소장 |
| 30 | Heif M, Yen RD, Shah RJ. ERCP with probe-based confocal laser endomicroscopy for the evaluation of dominant biliary stenoses in primary sclerosing cholangitis patients. Dig Dis Sci 2013;58:2068-2074. | 미소장 |
| 31 | Caillol F, Bories E, Autret A, et al. Evaluation of pCLE in the bile duct:final results of EMID study : pCLE: impact in the management of bile duct strictures. Surg Endosc 2015;29:2661-2668. | 미소장 |
| 32 | Slivka A, Gan I, Jamidar P, et al. Validation of the diagnostic accuracy of probe-based confocal laser endomicroscopy for the characterization of indeterminate biliary strictures: results of a prospective multicenter international study. Gastrointest Endosc 2015;81:282-290. | 미소장 |
| 33 | Dubow M, Tatman PD, Shah RJ. Individual probe based confocal laser endomicroscopy criteria in the analysis of indeterminate biliary strictures. Scand J Gastroenterol 2018;53:1358-1363. | 미소장 |
| 34 | Koda H, Hara K, Nozomi O, et al. High-resolution probe-based confocal laser endomicroscopy for diagnosing biliary diseases. Clin Endosc 2021;54:924-929. | 미소장 |
| 35 | Konda VJA, Meining A, Jamil LH, et al. A pilot study of in vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy under endosonographic guidance. Endoscopy 2013;45:1006-1013. | 미소장 |
| 36 | Nakai Y, Iwashita T, Park DH, Samarasena JB, Lee JG, Chang KJ. Diagnosis of pancreatic cysts: EUS-guided, through-the-needle confocal laser-induced endomicroscopy and cystoscopy trial: DETECT study. Gastrointest Endosc 2015;81:1204-1214. | 미소장 |
| 37 | Napoléon B, Lemaistre A-I, Pujol B, et al. A novel approach to the diagnosis of pancreatic serous cystadenoma: needle-based confocal laser endomicroscopy. Endoscopy 2015;47:26-32. | 미소장 |
| 38 | Krishna SG, Hart PA, Malli A, et al. Endoscopic ultrasound-guided confocal laser endomicroscopy increases accuracy of differentiation of pancreatic cystic lesions. Clin Gastroenterol Hepatol 2020;18:432-440. e6. | 미소장 |
| 39 | Keane MG, Wehnert N, Perez-Machado M, et al. A prospective trial of CONfocal endomicroscopy in CYSTic lesions of the pancreas: CONCYST-01. Endosc Int Open 2019;7:E1117-E1122. | 미소장 |
| 40 | Krishna SG, Hart PA, DeWitt JM, et al. EUS-guided confocal laser endomicroscopy:prediction of dysplasia in intraductal papillary mucinous neoplasms (with video). Gastrointest Endosc 2020;91:551-563.e5. | 미소장 |
| 41 | Hao S, Ding W, Jin Y, et al. Appraisal of EUS-guided needle-based confocal laser endomicroscopy in the diagnosis of pancreatic lesions: a single Chinese center experience. Endosc Ultrasound 2020;9:180-186. | 미소장 |
| 42 | Chin YK, Wu CCH, Tan DMY. The role of needle-based confocal laser endomicroscopy in the evaluation of pancreatic cystic lesions: a systematic review. Clin Endosc 2021;54:38-47. | 미소장 |
| 43 | Giovannini M, Caillol F, Monges G, et al. Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy in solid pancreatic masses. Endoscopy 2016;48:892-898. | 미소장 |
| 44 | Orr J, Lockwood R, Roberts J, Shi C, Yachimski P. EUS and confocal endomicroscopic diagnosis of pancreatic acinar cell cystadenoma. Gastrointest Endosc 2018;88:769-770. | 미소장 |
| 45 | ASGE Standards of Practice Committee, Muthusamy VR, Chandrasekhara V, et al. The role of endoscopy in the diagnosis and treatment of cystic pancreatic neoplasms. Gastrointest Endosc 2016;84:1-9. | 미소장 |
| 46 | European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut 2018;67:789-804. | 미소장 |
| 47 | Larghi A, Crinò SF, Napoleon B. Pancreatic cystic lesions: time to move to 19-gauge needle with EUS-guided microforceps biopsy or needle-based confocal laser endomicroscopy. Gastrointest Endosc 2020;92:222. | 미소장 |
| 48 | Bhutani MS, Koduru P, Joshi V, et al. EUS-guided needle-based confocal laser endomicroscopy: a novel technique with emerging applications. Gastroenterol Hepatol (NY) 2015;11:235-240. | 미소장 |
| 49 | Yang D, Samarasena JB, Jamil LH, et al. Endoscopic ultrasound-guided through-the-needle microforceps biopsy in the evaluation of pancreatic cystic lesions: a multicenter study. Endosc Int Open 2018;6:E1423-E1430. | 미소장 |
| 50 | Karia K, Waxman I, Konda VJ, et al. Needle-based confocal endomicroscopy for pancreatic cysts: the current agreement in interpretation. Gastrointest Endosc 2016;83:924-927. | 미소장 |
| 51 | Talreja JP, Sethi A, Jamidar PA, et al. Interpretation of probe-based confocal laser endomicroscopy of indeterminate biliary strictures: is there any interobserver agreement? Dig Dis Sci 2012;57:3299-3302. | 미소장 |
| 52 | Aubreville M, Stoeve M, Oetter N, et al. Deep learning-based detection of motion artifacts in probe-based confocal laser endomicroscopy images. Int J Comput Assist Radiol Surg 2019;14:31-42. | 미소장 |
| 53 | Rasti P, Wolf C, Dorez H, et al. Machine learning-based classification of the health state of mice colon in cancer study from confocal laser endomicroscopy. Sci Rep 2019;9:20010. | 미소장 |
*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
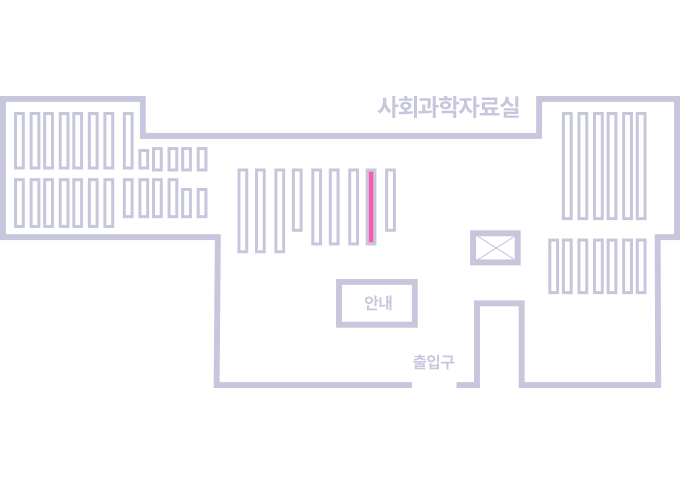
도서위치안내: 정기간행물실(524호) / 서가번호: 국내16
2021년 이전 정기간행물은 온라인 신청(원문 구축 자료는 원문 이용)
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.