권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
Contents
Noninvasive assessment of hepatic steatosis using a pathologic reference standard : comparison of CT, MRI, and US-based techniques / Jae Seok Bae ; Dong Ho Lee ; Kyung-Suk Suh ; Haeryoung Kim ; Kyung Bun Lee ; Jae Young Lee ; Joon Koo Han 1
[요약] 1
Introduction 2
Materials and Methods 2
Results 5
Discussion 7
Author Contributions 9
Supplementary Material 9
References 10
| 번호 | 참고문헌 | 국회도서관 소장유무 |
|---|---|---|
| 1 | World J Gastroenterol. 2019 Oct 28;25(40):6053-6062 | 미소장 |
| 2 | AJR Am J Roentgenol. 2017 Jan;208(1):92-100 | 미소장 |
| 3 | J Ultrasound Med. 2021 Jul;40(7):1325-1332 | 미소장 |
| 4 | Ann Surg. 2013 May;257(5):922-8 | 미소장 |
| 5 | Eur Radiol. 2020 Apr;30(4):2293-2301 | 미소장 |
| 6 | Clin Mol Hepatol. 2017 Dec;23(4):290-301 | 미소장 |
| 7 | Eur Radiol. 2019 Dec;29(12):6499-6507 | 미소장 |
| 8 | World J Gastroenterol. 2016 Jan 28;22(4):1664-73 | 미소장 |
| 9 | J Hepatol. 2014 May;60(5):1026-31 | 미소장 |
| 10 | Ultrasound Med Biol. 2019 Jun;45(6):1407-1416 | 미소장 |
| 11 | J Hepatol. 2017 Sep;67(3):577-584 | 미소장 |
| 12 | Ultrasound Med Biol. 2010 Nov;36(11):1825-35 | 미소장 |
| 13 | Clin Gastroenterol Hepatol. 2021 Apr;19(4):797-805.e7 | 미소장 |
| 14 | Ultrasonography. 2020 Apr;39(2):121-129 | 미소장 |
| 15 | Ultrasound Med Biol. 2019 Oct;45(10):2679-2687 | 미소장 |
| 16 | Lancet Gastroenterol Hepatol. 2020 Nov;5(11):996-1007 | 미소장 |
| 17 | Hepatology. 2005 Jun;41(6):1313-21 | 미소장 |
| 18 | JAMA. 2020 Mar 24;323(12):1175-1183 | 미소장 |
| 19 | Transplantation. 2013 Feb 15;95(3):501-6 | 미소장 |
| 20 | Radiology. 2018 Feb;286(2):486-498 | 미소장 |
| 21 | J Hepatol. 2010 Apr;52(4):579-85 | 미소장 |
| 22 | Eur Radiol. 2021 Aug;31(8):5802-5811 | 미소장 |
| 23 | Am J Gastroenterol. 2007 Feb;102(2):399-408 | 미소장 |
| 24 | J Hepatol. 2013 May;58(5):1007-19 | 미소장 |
| 25 | Liver Int. 2021 Jan;41(1):81-90 | 미소장 |
| 26 | Clin Transl Gastroenterol. 2019 Oct;10(10):e00081 | 미소장 |
| 27 | Genet Med. 2016 Jun;18(6):618-26 | 미소장 |
| 28 | J Hepatol. 2009 Dec;51(6):1061-7 | 미소장 |
| 29 | Radiology. 2010 Jul;256(1):159-68 | 미소장 |
| 30 | Radiology. 2020 Sep;296(3):532-540 | 미소장 |
| 31 | Radiology. 2006 Apr;239(1):105-12 | 미소장 |
| 32 | Radiology. 2019 Mar;290(3):682-690 | 미소장 |
| 33 | J Gastrointest Surg. 2003 Dec;7(8):1034-44 | 미소장 |
| 34 | Gastroenterology. 2019 May;156(6):1717-1730 | 미소장 |
| 35 | Am J Gastroenterol. 2018 Nov;113(11):1649-1659 | 미소장 |
| 36 | Hepatology. 2020 Nov;72(5):1605-1616 | 미소장 |
| 37 | Gastroenterology. 2016 Mar;150(3):626-637.e7 | 미소장 |
| 38 | Obes Rev. 2004 Feb;5(1):27-42 | 미소장 |
| 39 | Eur Radiol. 2019 Aug;29(8):4427-4435 | 미소장 |
*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
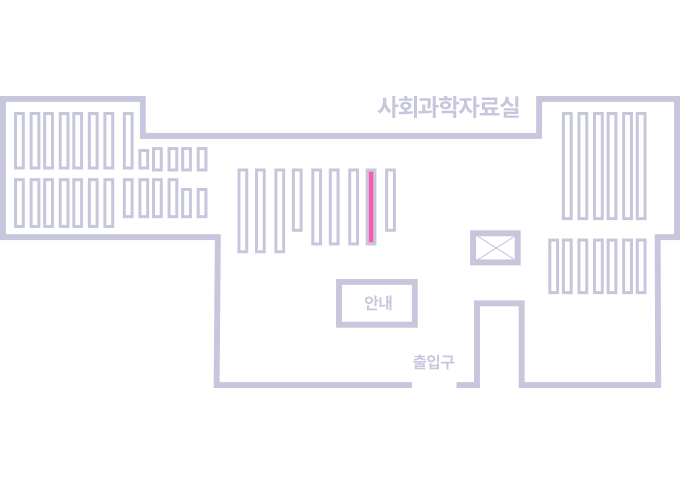
도서위치안내: 정기간행물실(524호) / 서가번호: 국내18
2021년 이전 정기간행물은 온라인 신청(원문 구축 자료는 원문 이용)
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.