권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
배경: 균혈증은 치사율이 30-40%에 이르며 환자에게 치명적일 수 있다. 타임 랩스 촬영 기술을 기반으로 한 QMAC-dRAST 시스템(QuantaMatrix, Republic of Korea)은 기존 장비보다 신속하게 항균제 감수성 검사(antimicrobial susceptibility testing, AST) 결과를 보고할 수 있다. 본 연구에서는 양성 임상 혈액 배양 검체에 대한 QMAC-dRAST의 성능을 평가하였다.
방법: 총 204개의 균주가 양성 혈액 배양에서 수집되었고 그 중 104개가 그람양성균, 100개가 그람음성균으로, Staphylococcus spp., Enterococcus spp., Enterobacteriaceae, Pseudomonas aeruginosa, 그리고 Acinetobacter spp.가 포함되었다. AST 결과 해석 알고리즘(AST 알고리즘) 개선 전후로 67개의 그람양성균과 72개의 그람음성균을 검사하였고 그 결과를 비교하였다. 최종 검사에서는 37개의 그람양성균과 28개의 그람음성균이 추가되었고, 최종적으로 204개의 균주를 이용하여 QMAC-dRAST와 Vitek 2 사이의 일치율을 분석하였다. QMAC-dRAST와 Vitek 2 사이의 불일치 AST 결과를 해결하기 위해, 미량액체배지희석법을 시행하였다.
결과: 그람양성균 67개와 그람음성균 72개를 이용한 1, 2차 시험에서 AST 알고리즘을 개선한 결과, QMAC-dRAST와 Vitek 2의 categorical agreement가 각각 92.7%, 96.2%에서 94.3%, 96.5%로 증가하였다. 204개의 모든 균주 대상으로는 각각 94.5%, 95.4%의 categorical agreement와, 4.8%, 0.6%의 very major error와, 2.5%, 2.0%의 major error가 관찰되었으며, minor error는 2.1%, 3.0%로 나타났다.
결론: QMAC-dRAST 시스템은 신뢰할 만한 성능과 기존 방법보다 빨리 AST 결과를 보고할 수 있는 장점을 가지고 있다. 이 시스템은 향후 AST 알고리즘을 추가적으로 개선하여 기존 AST 시스템과 더욱 높은 일치율을 보여줄 것이다.
Background: Bacteremia is life-threatening to patients, with a case fatality rate of 30–40%. The QMAC-dRAST system (QuantaMatrix, Republic of Korea), which is based on time-lapse imaging technology, can generate antimicrobial susceptibility testing (AST) results earlier than conventional equipment. Here, we evaluated the performance of QMAC-dRAST for positive blood culture samples.
Methods: In total, 204 isolates were collected from positive blood cultures, with 104 Gram-positive cocci (GPC) and 100 Gram-negative rods (GNR), including Staphylococcus spp., Enterococcus spp., Enterobacteriaceae, Pseudomonas aeruginosa, and Acinetobacter spp. Before and after improvement of the AST algorithm, 67 GPC isolates and 72 GNR isolates were tested and their results were compared. In the final test, 37 GPC and 28 GNR were added, and the agreement rates between QMAC-dRAST and Vitek 2 were analyzed using 204 samples. To resolve discrepant AST results between two systems, broth microdilution tests were performed.
Results: In the first and second tests with 67 GPC and 72 GNR, the categorical agreement (CA) between QMAC-dRAST and Vitek 2 was increased from 92.7% and 96.2% to 94.3% and 96.5% by updating the AST algorithm, respectively. For all 204 samples, the agreement rates were 94.5% and 95.4% for CA; 4.8% and 0.6% for very major errors; 2.5% and 2.0% for major errors; and 2.1% and 3.0% for minor errors.
Conclusions: The QMAC-dRAST system has reliable performance and the advantage of faster AST reporting than conventional methods. This system will demonstrate more acceptable agreement rates with conventional AST systems in the future by improving AST algorithms.| 번호 | 참고문헌 | 국회도서관 소장유무 |
|---|---|---|
| 1 | Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest 2000;118:146-55. | 미소장 |
| 2 | Leibovici L, Samra Z, Konigsberger H, Drucker M, Ashkenazi S, Pitlik SD. Long-term survival following bacteremia or fungemia. JAMA 1995;274:807-12. | 미소장 |
| 3 | Lee Y, Kim YA, Song W, Lee H, Lee HS, Jang SJ, et al. Recent trends in antimicrobial resistance in intensive care units in Korea. Korean J Nosocomial Infect Control 2013;19:29-36. | 미소장 |
| 4 | Liu C, Yoon EJ, Kim D, Shin JH, Shin JH, Shin KS, et al. Antimicrobial resistance in South Korea: A report from the Korean global antimicrobial resistance surveillance system (Kor-GLASS) for 2017. Infect Chemother 2019;25:845-59. | 미소장 |
| 5 | Seo YH, Jeong JH, Lee HT, Kwoun WJ, Park PW, Ahn JY, et al. Analysis of blood culture data at a tertiary university hospital, 2006-2015. Ann Clin Microbiol 2017;20:35-41. | 미소장 |
| 6 | Park ES, Jin HY, Jeong SY, Kweon OM, Yoo SY, Park SY, et al. Healthcare-associated infection surveillance in small and medium sized hospitals. Korean J Nosocomial Infect Control 2011;16:54-62. | 미소장 |
| 7 | Lee HG, Jang J, Choi JE, Chung DC, Han JW, Woo H, et al. Blood stream infections in patients in the burn intensive care unit. Infect Chemother 2013;45:194-201. | 미소장 |
| 8 | van Belkum A, Burnham CD, Rossen JWA, Mallard F, Rochas O, Dunne WM Jr. Innovative and rapid antimicrobial susceptibility testing systems. Nat Rev Microbiol 2020:18;299-311. | 미소장 |
| 9 | Quesada MD, Giménez M, Molinos S, Fernández G, Sánchez MD, Rivelo R, et al. Performance of VITEK-2 Compact and overnight MicroScan panels for direct identification and susceptibility testing of Gram-negative bacilli from positive FAN BacT/ALERT blood culture bottles. Clin Microbiol Infect 2010;16:137-40. | 미소장 |
| 10 | Choi J, Jeong HY, Lee GY, Han S, Han S, Jin B, et al. Direct, rapid antimicrobial susceptibility test from positive blood cultures based on microscopic imaging analysis. Sci Rep 2017;7:1148. | 미소장 |
| 11 | Choi J, Jung YG, Kim J, Kim S, Jung Y, Na H, et al. Rapid antibiotic susceptibility testing by tracking single cell growth in a microfluidic agarose channel system. Lab Chip 2013;13:280-7. | 미소장 |
| 12 | Wang HY, Uh Y, Kim S, Lee H. Quantamatrix Multiplexed Assay Platform system for direct detection of bacteria and antibiotic resistance determinants in positive blood culture bottles. Clin Microbiol Infect 2017;23:333.e1-7. | 미소장 |
| 13 | Kim JH, Kim TS, Song SH, Choi J, Han S, Kim DY, et al. Direct rapid antibiotic susceptibility test (dRAST) for blood culture and its potential usefulness in clinical practice. J Med Microbiol 2018;67:325-31. | 미소장 |
| 14 | Grohs P, Rondinaud E, Fourar M, Rouis K, Mainardi JL, Podglajen I. Comparative evaluation of the QMAC-dRAST V2.0 system for rapid antibiotic susceptibility testing of Gram-negative blood culture isolates. J Microbiol Methods 2020;172:105902. | 미소장 |
| 15 | Huh HJ, Song DJ, Shim HJ, Kwon WK, Park MS, Ryu MR, et al. Performance evaluation of the QMAC-dRAST for staphylococci and enterococci isolated from blood culture: a comparative study of performance with the VITEK-2 system. J Antimicrob Chemother 2018;73:1267-71. | 미소장 |
| 16 | Kim H, Jeong HY, Han S, Han S, Choi J, Jin B, et al. Clinical Evaluation of QMAC-dRAST for Direct and Rapid Antimicrobial Susceptibility Test with Gram-Positive Cocci from Positive Blood Culture Bottles. Ann Clin Microbiol 2018;21:12-9. | 미소장 |
| 17 | Clinical and Laboratory Standards Institute. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. 11th ed. CLSI standard M07. Wayne, PA: Clinical and Laboratory Standards Institute, 2018. | 미소장 |
| 18 | U.S. Department of Health and Human Services Food and Drug Administration Center for Devices and Radiological Health. Antimicrobial Susceptibility Test (AST) Systems - Class II special controls guidance for Industry and FDA. https://www.fda.gov/medical-devices/guidance-documents-medical-devices-and-radiation-emitting-products/antimicrobial-susceptibility-test-ast-systems-class-ii-special-controls-guidance-industry-and-fda#1 (Updated on Feb 2018). | 미소장 |
| 19 | van Belkum A, Burnham CD, Rossen JWA, Mallard F, Rochas O, Dunne WM Jr. Innovative and rapid antimicrobial susceptibility testing systems. Nat Rev Microbiol 2020;18:299-311. | 미소장 |
| 20 | Jin WY, Jang SJ, Lee MJ, Park G, Kim MJ, Kook JK, et al. Evaluation of VITEK 2, MicroScan, and Phoenix for identification of clinical isolates and reference strains. Diagn Microbiol Infect Dis 2011;70:442-7. | 미소장 |
| 21 | Banerjee R and Humphries R. Rapid antimicrobial susceptibility testing methods for blood cultures and their clinical impact. Front Med (Lausanne) 2021;8:635831. | 미소장 |
| 22 | Gaynes R and Edwards JR. Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis 2005;41:848-54. | 미소장 |
| 23 | Klevens RM, Edwards JR, Tenover FC, McDonald LC, Horan T, Gaynes R, et al. Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992–2003. Clin Infect Dis 2006;42:389-91. | 미소장 |
| 24 | Ramsey AM and Zilberberg MD. Secular trends of hospitalization with vancomycin-resistant enterococcus infection in the United States, 2000–2006. Infect Control Hosp Epidemiol 2009;30:184-6. | 미소장 |
| 25 | Lee K. Trend of bacterial resistance for the past 50 years in Korea and future perspectives-gram-negative bacteria. Infect Chemother 2011;43:458-67. | 미소장 |
*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
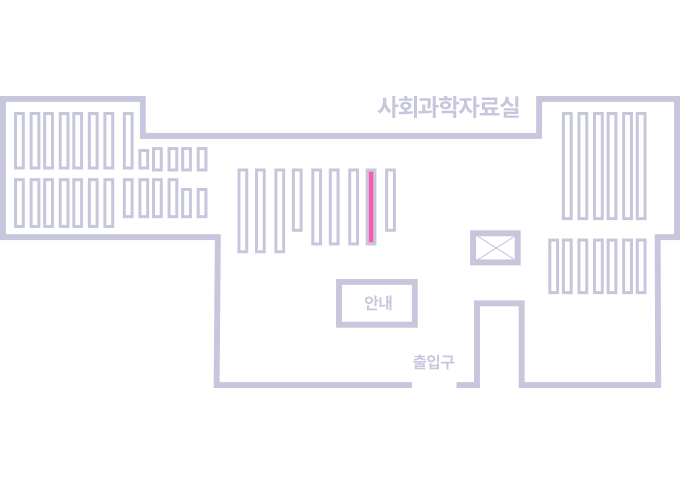
도서위치안내: / 서가번호:
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.