권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
OBJECTIVES: Certain studies have reported that handgrip strength (HGS) is associated with metabolic health risks in children and adolescents, and some studies have suggested HGS thresholds for identifying poor metabolic health. Therefore, we aimed to determine the HGS thresholds associated with metabolic syndrome (MetS) in children and adolescents through a systematic review.
METHODS: We searched 3 electronic databases from their inception until October 2023 to identify original papers that focused on children and adolescents and assessed their risks of MetS according to specific HGS values. Studies were selected for inclusion through a planned screening process based on specific criteria. The Quality Assessment Tool for Diagnostic Accuracy Studies version 2 (QUADAS-2) was used to evaluate quality, and a meta-analysis was performed using the diagmeta R package to suggest the optimal thresholds.
RESULTS: From the search, 8 studies were selected for this systematic review. For detecting MetS risk, the optimal threshold for HGS (defined as relative HGS by adjusting for body mass) was found to be 0.422, with a sensitivity of 76.7% (95% confidence interval [CI], 64.0 to 85.8) and a specificity of 62.9% (95% CI, 56.9 to 68.5). The stratification analysis by sex resulted in optimal thresholds of 0.416 for boys and 0.376 for girls. Additionally, when the data were stratified by age, the thresholds were 0.356 for children and 0.416 for adolescents.
CONCLUSIONS: Our results provide practical information for detecting high-risk groups and encouraging strength-related activities that may reduce the risk of MetS in children and adolescents.| 번호 | 참고문헌 | 국회도서관 소장유무 |
|---|---|---|
| 1 | Chang TH, Chen YC, Chen WY, Chen CY, Hsu WY, Chou Y, et al. Weight gain associated with COVID-19 lockdown in children and adolescents: a systematic review and meta-analysis. Nutrients 2021;13:3668. https://doi.org/10.3390/nu13103668 | 미소장 |
| 2 | Lange SJ, Kompaniyets L, Freedman DS, Kraus EM, Porter R; DNP3, et al. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2-19 years - United States, 2018-2020. MMWR Morb Mortal Wkly Rep 2021;70:1278-1283. https://doi.org/10.15585/mmwr.mm7037a3 | 미소장 |
| 3 | Woolford SJ, Sidell M, Li X, Else V, Young DR, Resnicow K, et al. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA 2021;326:1434-1436. https://doi.org/10.1001/jama.2021.15036 | 미소장 |
| 4 | Fäldt A, Nejat S, Edvinsson Sollander S, Durbeej N, Holmgren A. Increased incidence of overweight and obesity among preschool Swedish children during the COVID-19 pandemic. Eur J Public Health 2023;33:127-131. https://doi.org/10.1093/eurpub/ckac181 | 미소장 |
| 5 | Noubiap JJ, Nansseu JR, Lontchi-Yimagou E, Nkeck JR, Nyaga UF, Ngouo AT, et al. Global, regional, and country estimates of metabolic syndrome burden in children and adolescents in 2020: a systematic review and modelling analysis. Lancet Child Adolesc Health 2022;6:158-170. https://doi.org/10.1016/S2352-4642(21)00374-6 | 미소장 |
| 6 | Castro-Piñero J, Laurson KR, Artero EG, Ortega FB, Labayen I, Ruperez AI, et al. Muscle strength field-based tests to identify European adolescents at risk of metabolic syndrome: the HELENA study. J Sci Med Sport 2019;22:929-934. https://doi.org/10. 1016/j.jsams.2019.04.008 | 미소장 |
| 7 | Peterson MD, Zhang P, Saltarelli WA, Visich PS, Gordon PM. Low muscle strength thresholds for the detection of cardiometabolic risk in adolescents. Am J Prev Med 2016;50:593-599. https://doi.org/10.1016/j.amepre.2015.09.019 | 미소장 |
| 8 | Ramírez-Vélez R, Peña-Ibagon JC, Martínez-Torres J, Tordecilla-Sanders A, Correa-Bautista JE, Lobelo F, et al. Handgrip strength cutoff for cardiometabolic risk index among Colombian children and adolescents: the FUPRECOL Study. Sci Rep 2017;7:42622. https://doi.org/10.1038/srep42622 | 미소장 |
| 9 | de Lima TR, Martins PC, Torre GL, Mannocci A, Silva KS, Silva DA. Association between muscle strength and risk factors for metabolic syndrome in children and adolescents: a systematic review. J Pediatr Endocrinol Metab 2020;34:1-12. https://doi.org/10.1515/jpem-2020-0135 | 미소장 |
| 10 | Fraser BJ, Rollo S, Sampson M, Magnussen CG, Lang JJ, Tremblay MS, et al. Health-related criterion-referenced cut-points for musculoskeletal fitness among youth: a systematic review. Sports Med 2021;51:2629-2646. https://doi.org/10.1007/s40279-021-01524-8 | 미소장 |
| 11 | Wen Y, Liu T, Ma C, Fang J, Zhao Z, Luo M, et al. Association between handgrip strength and metabolic syndrome: a meta-analysis and systematic review. Front Nutr 2022;9:996645. https://doi.org/10.3389/fnut.2022.996645 | 미소장 |
| 12 | Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016;5:210. https://doi.org/10.1186/s13643-016-0384-4 | 미소장 |
| 13 | Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529-536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009 | 미소장 |
| 14 | Kaur G, Lakshmi PV, Rastogi A, Bhansali A, Jain S, Teerawattananon Y, et al. Diagnostic accuracy of tests for type 2 diabetes and prediabetes: a systematic review and meta-analysis. PLoS One 2020;15:e0242415. https://doi.org/10.1371/journal.pone.0242415 | 미소장 |
| 15 | Ko DH, Kim YK. The prevalence of metabolic syndrome according to grip strength in teenagers. Children (Basel) 2021;8:108. https://doi.org/10.3390/children8020108 | 미소장 |
| 16 | Choi EY. Relationship of handgrip strength to metabolic syndrome among Korean adolescents 10-18 years of age: results from the Korean National Health and Nutrition Examination Survey 2014-18. Metab Syndr Relat Disord 2021;19:93-99. https://doi.org/10.1089/met.2020.0074 | 미소장 |
| 17 | Lee CH, Lee JH, Jeong YW, Koh H, Kang Y. Handgrip strength cutoff value among Korean adolescents with metabolic syndrome components: Korean National Health and Nutrition Examination Survey data 2014-2017. Metab Syndr Relat Disord 2022;20:584-591. https://doi.org/10.1089/met.2022.0051 | 미소장 |
| 18 | Jung HW, Lee J, Kim J. Handgrip strength is associated with metabolic syndrome and insulin resistance in children and adolescents: analysis of Korea National Health and Nutrition Examination Survey 2014-2018. J Obes Metab Syndr 2022;31:334-344. https://doi.org/10.7570/jomes22053 | 미소장 |
| 19 | Steinhauser S, Schumacher M, Rücker G. Modelling multiple thresholds in meta-analysis of diagnostic test accuracy studies. BMC Med Res Methodol 2016;16:97. https://doi.org/10.1186/s12874-016-0196-1 | 미소장 |
| 20 | Castro-Piñero J, Perez-Bey A, Cuenca-Garcia M, Cabanas-Sanchez V, Gómez-Martínez S, Veiga OL, et al. Muscle fitness cut points for early assessment of cardiovascular risk in children and adolescents. J Pediatr 2019;206:134-141. https://doi.org/10.1016/j.jpeds.2018.10.026 | 미소장 |
| 21 | López-Gil JF, Weisstaub G, Ramírez-Vélez R, García-Hermoso A. Handgrip strength cut-off points for early detection of cardiometabolic risk in Chilean children. Eur J Pediatr 2021;180:3483-3489. https://doi.org/10.1007/s00431-021-04142-8 | 미소장 |
| 22 | Fraser BJ, Huynh QL, Schmidt MD, Dwyer T, Venn AJ, Magnussen CG. Childhood muscular fitness phenotypes and adult metabolic syndrome. Med Sci Sports Exerc 2016;48:1715-1722. https://doi.org/10.1249/MSS.0000000000000955 | 미소장 |
| 23 | Zaqout M, Michels N, Bammann K, Ahrens W, Sprengeler O, Molnar D, et al. Influence of physical fitness on cardio-metabolic risk factors in European children. The IDEFICS study. Int J Obes (Lond) 2016;40:1119-1125. https://doi.org/10.1038/ijo.2016.22 | 미소장 |
| 24 | Huang TT, Ball GD, Franks PW. Metabolic syndrome in youth: current issues and challenges. Appl Physiol Nutr Metab 2007;32:13-22. https://doi.org/10.1139/h06-094 | 미소장 |
| 25 | Jiménez-Pavón D, Ortega FB, Valtueña J, Castro-Piñero J, Gómez-Martínez S, Zaccaria M, et al. Muscular strength and markers of insulin resistance in European adolescents: the HELENA Study. Eur J Appl Physiol 2012;112:2455-2465. https://doi.org/10.1007/s00421-011-2216-5 | 미소장 |
| 26 | Rioux BV, Kuwornu P, Sharma A, Tremblay MS, McGavock JM, Sénéchal M. Association between handgrip muscle strength and cardiometabolic z-score in children 6 to 19 years of age: results from the Canadian health measures survey. Metab Syndr Relat Disord 2017:379-384. https://doi.org/10.1089/met.2016.0147 | 미소장 |
| 27 | Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr Diabetes 2007;8:299-306. https://doi.org/10.1111/j.1399-5448.2007.00271.x | 미소장 |
| 28 | Choi EJ, Lee HA, Park B, Park B, Kim HS, Hong YS, et al. Trajectory patterns for continuous metabolic syndrome score in childhood and the cardiovascular risk in adolescence. Sci Rep 2021;11:22564. https://doi.org/10.1038/s41598-021-01566-y | 미소장 |
| 29 | Wind AE, Takken T, Helders PJ, Engelbert RH. Is grip strength a predictor for total muscle strength in healthy children, adolescents, and young adults? Eur J Pediatr 2010;169:281-287. https://doi.org/10.1007/s00431-009-1010-4 | 미소장 |
| 30 | Mutalib SA, Mace M, Seager C, Burdet E, Mathiowetz V, Goldsmith N. Modernising grip dynamometry: inter-instrument reliability between GripAble and Jamar. BMC Musculoskelet Disord 2022;23:80. https://doi.org/10.1186/s12891-022-05026-0 | 미소장 |
| 31 | Gąsior JS, Pawłowski M, Jeleń PJ, Rameckers EA, Williams CA, Makuch R, et al. Test-retest reliability of handgrip strength measurement in children and preadolescents. Int J Environ Res Public Health 2020;17:8026. https://doi.org/10.3390/ijerph17218026 | 미소장 |
| 32 | Trajković N, Rančić D, Ilić T, Herodek R, Korobeynikov G, Pekas D. Measuring handgrip strength in school children: inter-instrument reliability between Takei and Jamar. Sci Rep 2024;14:1074. https://doi.org/10.1038/s41598-024-51368-1 | 미소장 |
| 33 | World Health Organization. Physical activity; 2022 [cited 2024 Jan 6]. Available from: https://www.who.int/news-room/fact-sheets/detail/physical-activity | 미소장 |
| 34 | Myers J, Kokkinos P, Nyelin E. Physical activity, cardiorespiratory fitness, and the metabolic syndrome. Nutrients 2019;11:1652. https://doi.org/10.3390/nu11071652 | 미소장 |
| 35 | Wu J, Yang Y, Yu H, Li L, Chen Y, Sun Y. Comparative effectiveness of school-based exercise interventions on physical fitness in children and adolescents: a systematic review and network meta-analysis. Front Public Health 2023;11:1194779. https://doi.org/10.3389/fpubh.2023.1194779 | 미소장 |
| 36 | World Health Organization. WHO guidelines on physical activity and sedentary behavior; 2020 [cited 2024 Jan 6]. Available from: https://www.who.int/publications/i/item/9789240015128 | 미소장 |
| 37 | World Health Organization. Physical activity fact sheet; 2021 [cited 2024 Jan 6]. Available from: https://iris.who.int/handle/10665/346252 | 미소장 |
| 38 | Merlo CL, Jones SE, Michael SL, Chen TJ, Sliwa SA, Lee SH, et al. Dietary and physical activity behaviors among high school students - Youth Risk Behavior Survey, United States, 2019. MMWR Suppl 2020;69:64-76. https://doi.org/10.15585/mmwr.su6901a8 | 미소장 |
| 39 | Xin F, Zhu Z, Chen S, Chen H, Hu X, Ma X, et al. Prevalence and correlates of meeting the muscle-strengthening exercise recommendations among Chinese children and adolescents: results from 2019 Physical Activity and Fitness in China-the Youth Study. J Sport Health Sci 2022;11:358-366. https://doi.org/10.1016/j.jshs.2021.09.010 | 미소장 |
| 40 | Seo YB, Oh YH, Yang YJ. Current status of physical activity in South Korea. Korean J Fam Med 2022;43:209-219. https://doi.org/10.4082/kjfm.22.0099 | 미소장 |
| 41 | Bozzola E, Barni S, Ficari A, Villani A. Physical activity in the COVID-19 era and its impact on adolescents’ well-being. Int J Environ Res Public Health 2023;20:3275. https://doi.org/10.3390/ijerph20043275 | 미소장 |
| 42 | Choi JE, Lee HA, Park SW, Lee JW, Lee JH, Park H, et al. Increase of prevalence of obesity and metabolic syndrome in children and adolescents in Korea during the COVID-19 pandemic: a cross-sectional study Using the KNHANES. Children (Basel) 2023;10:1105. https://doi.org/10.3390/children10071105 | 미소장 |
*표시는 필수 입력사항입니다.
| 전화번호 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
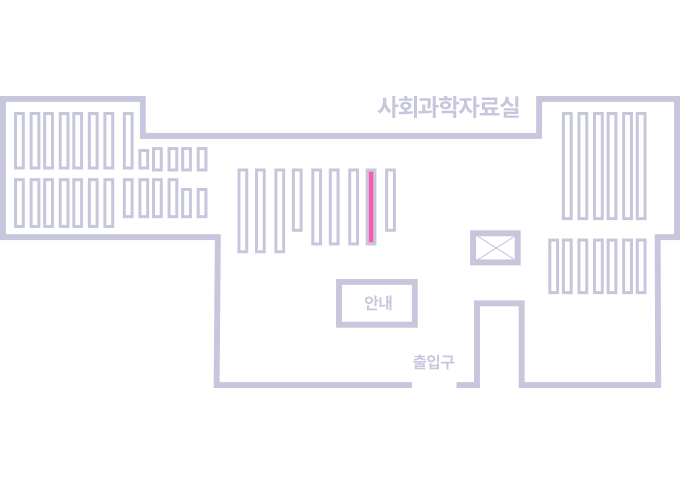
도서위치안내: / 서가번호:
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.