Ⅰ. 연구결과 요약문 5
Ⅱ. 정책연구용역사업 연구결과 7
1.1. 목표 7
1.2. 목표달성도 및 관련분야에 대한 기여도 8
2-1. 국외 기술 현황 9
2-2. 국내 기술 현황 9
3-1. 연구 내용 10
3-2. 추진전략 10
3-3. 연구 방법 11
4-1. 다양한 항진균제 내성 아스페르길루스 균주 확보 18
4-2. 항진균제 내성 아스페르길루스 균주의 감별 동정법 연구 19
4-3. 국내 항진균제 획득내성과 자연내성 아스페르길루스의 비교 분석 23
4-4. 국내 항진균제 내성 아스페르길루스 현황 제시 및 결과 활용 방안 도출 29
1. 항진균제 내성 아스페르길루스 균주의 감별 동정법 연구 35
2. 국내 아스페르길루스의 숨은 균종(Cryptic species) 분포와 내성 양상의 비교 분석 36
3. 국내 항진균제 내성 A. flavus 균주의 azole 내성기전과 클론 전파 양상 비교 분석 36
4. 국내 amphotericin B 내성 A. terreus 균주의 클론 전파 연구 37
5. 국내 항진균제 내성 결과 활용 방안 38
6.1. 연구성과 39
6.2. 활용계획(연구사업 종료 후) 40
9.1. 연구비 사용 내역 44
9.2. 연구분담표 44
표목차제3장 최종 연구내용 및 방법 11
Table 1. Epidemiological cutoff values (ECVs) for systemic antifungal agents and Aspergillus species determined by CLSI M38-A broth microdilution method 11
Table 2. Primers used sequencing for identification of Aspergillus species 12
Table 3. Primers design for Cyp51 gene sequencing of A. flavus 13
Table 4. Primers used for real-time reverse transcription polymerase chain reaction (RT-PCR) for quantification of gene expression of A. flavus 14
Table 5. Primers used for microsatellite typing of A flavus 15
Table 6. Primers design for Cyp51A gene sequencing of A. terreus 16
Table 7. Primers used for microsatellite typing of A terreus 16
제4장 최종 연구결과 18
Table 1. Distribution of antifungal minimal inhibitory concentrations (MICs) of 351 clinical isolates of Aspergillus species determined by the CLSI M38-A method 18
Table 2. Identification (ID) results by sequence analysis using ITS, D1/D2, and β-tubulin for 351 clinical isolates of Aspergillus species from 11 hospitals in Korea 19
Table 3. Identification (ID) results by sequence analysis and matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) for 346 clinical isolates of Aspergillus... 20
Table 4. Identification (ID) results by three sequence analysis for 48 clinical isolates of A. flavus / A. oryzae complex from 11 hospitals in Korea 21
Table 5. The results of antifungal susceptibility testing for four common Aspergillus species from 11 hospitals in Korea 21
Table 6. The results of antifungal susceptibility testing for cryptic species of Aspergillus species from 11 hospitals in Korea 22
Table 7. The results for CYP51 gene sequencing of A. flavus isolates with voriconazole resistance 24
Table 8. Polymorphisms in CYP51C in 47 clinical isolates of A. flavus complex according to voriconazole MICs 25
Table 9. Effect of an efflux pump inhibitors on the MIC of voriconazole for clinical isolates of A. flavus 25
Table 10. Expression of CYP51A, CYP51B, CYP51C, MDR1, MDR2, MDR4, Aflatrf, and Afmfs1 genes in clinical isolates of A. flavus 26
Table 11. Results of microsatellite typing of voriconazole resistant isolates of A. flavus 27
Table 12. The results for CYP51A gene sequencing for 4 clinical isolates of A. terreus with voriconazole MIC 2 ug/ml 28
Table 13. Results of antifungal susceptibility to amphotericin B and microsatellite typing in 25 clinical isolates of A. terreus 28
Table 14. Species distribution of cryptic and common species of Aspergillus isolates from clinical specimens from nine university hospitals in Korea 30
Table 15. The results of antifungal susceptibility testing for common and cryptic species of Aspergillus species from 11 hospitals in Korea 30
Table 16. Lists of Aspergillus isolates for the deposit in KCDC and their microbiological features 33
Table 17. Lists of Aspergillus isolates for the deposit in KCDC and their clinical features 33
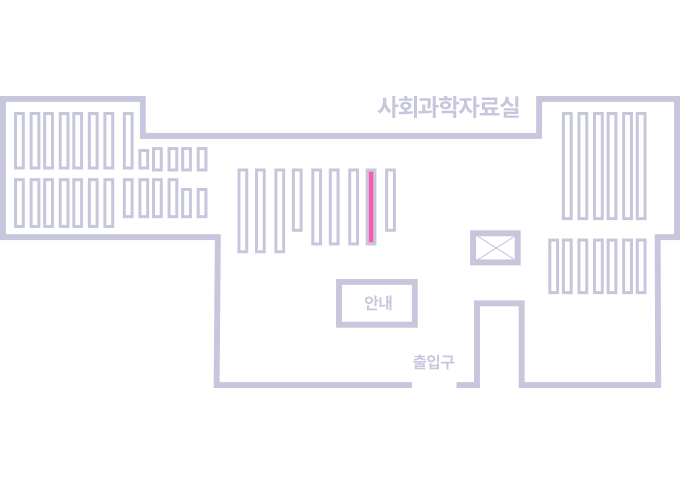
Figure 1. The proposed algorithm for identification of Aspergillus species of clinical relevance 32