권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
Title page
Contents
Abstract 3
1. Introduction 4
2. Background and study design 9
2.1. Setting 9
2.2. Participants 11
2.3. Intervention and randomization 12
2.4. Measurement and timing 13
2.5. Sample size and power 14
3. Estimation 15
3.1. Effects on enrollment, utilization and heath 15
3.2. Adverse selection 18
4. Results 20
4.1. Insurance enrollment 20
4.2. Insurance and hospital utilization 22
4.3. Health outcomes 25
4.4. Mechanisms through which insurance generates value 26
4.5. Adverse selection 27
5. Welfare analysis 29
5.1. Does offering (free) public insurance improve welfare? 29
5.2. What is the optimal public insurance premium? 38
6. Conclusion 41
References 43
Online Appendix 64
A. Methods 64
B. Welfare 68
C. Figures 73
D. Tables 80
Table 1. Characteristics of sample villages 54
Table 2. Household characteristics in different access-to-insurance conditions 55
Table 3. Trial design in each district 56
Table 4. Effects of premium & subsidy combinations on insurance enrollment 57
Table 5. Effect of premium & subsidy combinations on use of insurance and on hospital utilization (intent to treat estimates) 58
Table 6. Effect of insurance enrollment on use of insurance and on hospital utilization (complier average treatment effect) 59
Table 7. Number of significant health outcomes per category 60
Table 8. Effect of insurance access on total and out-of-pocket (OOP) medical expenditures (ITT) 61
Table 9. Enrollment by predicted spending 62
Table 10. Welfare calculations using four different measures of cost 63
Figure 1. Illustration of adverse selection 51
Figure 2. Inverse demand, cost and welfare calculations at midline 52
Figure 3. Inverse demand, cost and welfare calculations at endline 53
Table A.1. Outcomes measured by topic at midline (18 months post-intervention) and endline (3.5 years post-intervention) surveys 80
Table A.2. Effects of different premium & subsidy combinations on insurance enrollment 82
Table A.3. Enrollment by health (education, raven scores and risk aversion controlled) 83
Table A.4. Effect of insurance access on total and out-of-pocket (OOP) medical expenditures (CATE) 84
Table A.5. Effect of insurance enrollment on use of insurance for hospital care and on hospital utilization (CATE), by wealth of household 85
Table A.6. Reasons given for respondents' inability to use RSBY insurance card, by survey and utilization status 86
Table A.7. Effect of different premium & subsidy combinations on midline (18 mos.) health outcomes (intent to treat estimate) 87
Table A.8. Effect of different premium & subsidy combinations on endline (3.5 yrs.) health outcomes (intent to treat estimate) 90
Table A.9. Effect of insurance enrollment on midline (18 mos.) health outcomes (complier average treatment effect estimates) 95
Table A.10. Effect of insurance enrollment on endline (3.5 yrs.) health outcomes (complier average treatment effect estimates) 97
Table A.11. Number of significant health outcomes per category, without multiple testing adjustments 100
Table A.12. Estimates of demand and average cost using multiple different measures of cost 102
Table A.13. Sample size per insurance access group and response rates by survey and insurance access group 103
Table A.14. Respondent and response rate by module and insurance access group 104
Figure A.1. Balancing test result 73
Figure A.2. Estimates of total effects of insurance (CATE) on a randomly-selected set of health outcomes from midline (18 months) 74
Figure A.3. Estimates of total effects of insurance (CATE) on a randomly-selected set of health outcomes from endline (3.5 years) 75
Figure A.4. Quantile treatment effects on OOP spending 76
Figure A.5. Timeline of study 77
Figure A.6. Subject flowchart, with exclusions and attrition by endline 78
Figure A.7. Predicted medical expenditures 79
*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
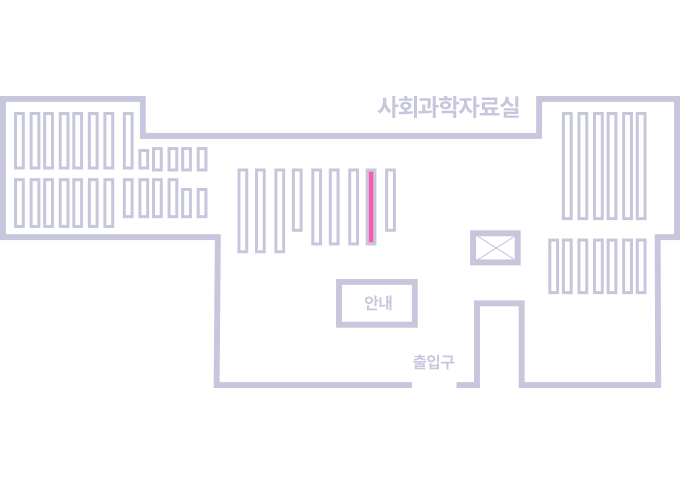
도서위치안내: / 서가번호:
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.