권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
Title page
Contents
Foreword 16
Preface 17
Acknowledgements 18
Overview 21
Abbreviations 40
Theoretical Framework 42
Chapter 1. Enhancing Human Capital and Boosting Productivity by Tackling Non-Communicable Diseases: Results of a research initiative 43
INTRODUCTION AND OVERVIEW 44
RESEARCH INPUTS AND POLICY DISCUSSIONS 46
RECOMMENDATIONS FOR KEY STAKEHOLDERS 68
CONCLUSIONS AND WAY FORWARD 70
REFERENCES 71
ANNEX 1.1. Toronto workshop agenda 72
ANNEX 1.2. Toronto workshop, list of participants 73
Chapter 2. Towards a Framework for Impact Pathways between NCDs, Human Capital and Healthy Longevity, Economic and Wellbeing Outcomes 74
INTRODUCTION 75
FACTORS IN DEVELOPING A FRAMEWORK, SOME DEFINITIONS, AND CROSS-CUTTING THEMES 76
HUMAN CAPITAL, GROWTH, AND COUNTRY WEALTH 81
INEQUALITY AND GENDER DIMENSIONS OF NCD AND HUMAN CAPITAL PATHWAYS 94
WELLBEING EFFECTS OF ADDRESSING NCDS 99
POLICIES AND INTERVENTIONS FOR NCDS AND HEALTHY LONGEVITY 101
CONCLUSION 107
REFERENCES 108
ANNEX 2.1 120
Economic Cost of Avoidable Mortality 124
Chapter 3. The Economic Value of Avoidable Mortality 125
INTRODUCTION 126
CONCEPTUAL FRAMEWORK 126
METHODS 128
RESULTS 131
DISCUSSION 140
CONCLUSION 143
DEDICATION 143
REFERENCES 143
Chapter 4. The Economic Value Associated with Avoidable Mortality: A systematic assessment by cause of death across world regions 145
INTRODUCTION 146
METHODS 147
RESULTS 150
DISCUSSION 160
REFERENCES 162
Chapter 5. Rates of progress in mortality decline, 2000-2019 164
INTRODUCTION 165
RATES OF PROGRESS OVER 2000-09 AND 2010-19 166
COUNTRIES' RATES OF PROGRESS DURING 2000-09 AND 2010-19 168
RATES OF PROGRESS IN CAUSE-SPECIFIC MORTALITY 171
COST OF SAVING A LIFE OVER TIME 173
REFERENCES 174
ANNEX 5.1. Interrupted time-series (ITS) analysis methodology 175
ANNEX 5.2. Methods used to estimate country performance during 2000 to 2019 176
ANNEX 5.3. Model using to estimate critical income 194
ANNEX REFERENCES 195
Behavior Change and Healthy Longevity 197
Chapter 6. Behavioral Aspects of Healthy Longevity 198
INTRODUCTION 199
A BEHAVIORAL SCIENCE FRAMEWORK FOR NCD POLICIES 201
NCD FORMATION: HEALTHY LIFESTYLE AND HABIT FORMATION 204
NCD DETECTION: SCREENING 208
NCD MANAGEMENT 211
RECOMMENDATIONS FOR A POLICY TOOLKIT 213
CONCLUSION 219
REFERENCES 220
ANNEX 6.1 226
Chapter 7. Taxation of harmful products, including tobacco, alcohol and sugar-sweetened beverages (SSBs), and related topics 227
INTRODUCTION: THE CONSUMPTION OF UNHEALTHY PRODUCTS AND THE HEALTHY LONGEVITY AGENDA 228
THE CONSUMPTION OF HARMFUL PRODUCTS AND THEIR EFFECTS 229
TAXATION: ECONOMIC RATIONALES AND EFFECTIVENESS 233
EFFECTIVENESS OF PRICE POLICIES 234
RELATED TOPICS 238
COMBINATION OF TAXES AND NON-PRICE INTERVENTIONS 240
CHALLENGES FROM THE INDUSTRY 240
CONCLUSIONS 244
REFERENCES 245
Gender and Aging 257
Chapter 8. Gender Gaps in Health and Well-Being of Older Adults: A review of the burden of non-communicable diseases and barriers to healthcare for women and men 258
INTRODUCTION 259
GENDER DIFFERENTIATED HEALTH OUTCOMES OF AGING POPULATIONS 263
AGING, GENDER, AND DEMAND FOR SERVICES 274
SUPPLY OF HEALTH AND CARE SERVICES FOR AGING POPULATIONS 277
WOMEN AS LONG-TERM CARE PROVIDERS 283
DISCUSSION 287
REFERENCES 290
ANNEX 8.1. Cancer mortality and prevalence by type for older women and men 298
Chapter 9. Gendered Responsibilities, Elderly Care, and Labor Supply: Evidence from four middle-income countries 300
INTRODUCTION 301
DATA 304
METHODOLOGY 305
RESULTS 305
HETEROGENEITY 316
ROBUSTNESS CHECK 317
CONCLUSION 319
REFERENCES 320
ANNEX 9.1 321
Long-term Care 327
Chapter 10. Health and Long-Term Care Needs in a Context of Rapid Population Aging 328
INTRODUCTION 329
MAIN TRENDS IN LONGEVITY 330
AGING, HEALTH, AND THE CHALLENGES FOR HEALTH CARE SYSTEMS 334
INCREASING RISK OF FUNCTIONAL DEPENDENCY AND CHALLENGES FOR LONG-TERM CARE SYSTEMS 355
FINAL REMARKS AND KEY POLICY CONSIDERATIONS 369
REFERENCES 372
CONSULTED SURVEYS AND DATABASES 381
Chapter 11. Demand for and Supply of Long-Term Care for Older Persons in Low- and Middle-Income Countries 382
INTRODUCTION 383
A DEMAND SIDE VIEW - CURRENT LTC LANDSCAPE IN MICS 384
A SUPPLY SIDE ASSESSMENT CURRENT LTC LANDSCAPE IN LMICS 397
DISCUSSION AND POLICY CONSIDERATIONS 404
REFERENCES 408
Social Protection and Jobs 411
Chapter 12. Exploring the labour market outcomes of the risk factors for non-communicable diseases: A systematic review 412
INTRODUCTION 413
METHODS 414
RESULTS 415
DISCUSSION 420
REFERENCES 422
ANNEX 12.1. Search strategy 425
Chapter 13. Productive Longevity: What can work in low- and middle-income countries? 426
INTRODUCTION 427
A GLOBAL POLICY AGENDA FOR AGING 428
WORK IN OLD AGE: SOME STYLIZED FACTS 430
WHAT HOLDS BACK PRODUCTIVE LONGEVITY? 436
PRODUCTIVE LONGEVITY: WHAT COULD WORK IN LMICS? 443
CONCLUSIONS: SOME META-LESSONS FOR PRODUCTIVE LONGEVITY 451
REFERENCES 452
ANNEX 13 458
Chapter 14. Adequacy Pensions and Access to Healthcare: Maintaining human capital during old age 459
INTRODUCTION 460
FINANCIAL PROTECTION 461
ACCESS TO HEALTH AND LONG-TERM CARE SERVICES 467
CONCLUSIONS 473
REFERENCES 473
Prioritizing Action 475
Chapter 15. Priority Setting for NCD Control and Health System Investments 476
INTRODUCTION 477
IDENTIFYING CANDIDATE NCD INTERVENTIONS 477
A FRAMEWORK FOR PRIORITIZING NCD INTERVENTIONS 479
POLICY IMPLICATIONS 484
REFERENCES 487
ANNEX 15.1. METHODS 489
Chapter 16. Control of Non-Communicable Diseases for Enhanced Human Capital: The case for whole-of-society action 491
INTRODUCTION 492
WHY FOCUS ON NCDs? 492
IMPACT OF THE COVID-19 PANDEMIC ON NCDs 498
RATIONALE FOR A WHOLE-OF-SOCIETY APPROACH TO NCDs 499
ENGAGING NON-STATE ACTORS (FOR-PROFIT AND NON-PROFIT) 506
WHAT HAS BEEN ACHIEVED SO FAR, AND WHAT HAVE WE LEARNED? 509
OPPORTUNITIES AND CHALLENGES FOR A WOS APPROACH: WHAT HAVE WE LEARNED? 524
THE WAY FORWARD 527
REFERENCES 528
Monitoring Indicators for Healthy Longevity 532
Chapter 17. Healthy Longevity Initiative: A performance dashboard for decision-making in low- and middle- income countries 533
INTRODUCTION 534
CONTEXTUALIZING DASHBOARDS FOR PERFORMANCE MONITORING AND STRATEGIC ACTION 535
A COMMON FRAMEWORK FOR HEALTHY LONGEVITY MEASUREMENT 535
CASE STUDIES: SIERRA LEONE, INDIA, AND COLOMBIA 538
DISCUSSION AND FUTURE DIRECTIONS 544
LIMITATIONS 548
CONCLUSION 549
REFERENCES 549
ANNEX 17.1. EXAMPLES OF DASHBOARDS FOR GLOBAL GOALS 552
ANNEX 17.2 560
Chapter 18. Assessing Human Capital, Non-communicable Diseases, and Healthy Longevity in Low- and Middle-Income Countries: Healthy longevity dashboard and the case for India 561
INTRODUCTION 562
METHODS 562
RESULTS 567
DISCUSSION 570
CONCLUSION 571
REFERENCES 572
ANNEX 18.1 573
ANNEX REFERENCES 574
Appendix 1: Acknowledgments by Chapter 576
Appendix 2: Workshops and Consultations 580
TABLE 1.1. Determinants of log adult (40q30) mortality and effect of intervention on adult mortality 58
TABLE 3.1. Gap between observed and frontier life expectancy at birth in years, 2000, 2019 and 2050, globally and by region 132
TABLE 3.2. Total mortality and percentage of mortality that is avoidable in 2019, globally and by region, for all ages and by age 133
TABLE 3.3. Value of avoidable mortality in 2019 globally and by region and age group 136
TABLE 4.1. Causes of death 148
TABLE 4.2. Economic value of avoidable mortality as a percentage of annual income by region and cause of death, for the years 2000, 2019, and 2030 153
TABLE 5.1. Results from interrupted time series analysis of the change in mortality rates (per 100,000 population) from 2000-10 to 2010-19, by country income,... 166
TABLE 5.2. Top 10 and worst 10 performance rankings among 71 LMICs in the rate of decline of mortality, by sex and age: 2000-10 and 2010-19 168
TABLE 5.3. Diseases and conditions showing country income level and age group with the fastest and slowest progress in mortality reduction, 2000-19 172
TABLE 5.4. Global maximum survival rates and critical income levels, 1990 to 2019 174
TABLE 5.5. Top five LMICs with the lowest critical income for ages under 15 years, 15-49 years, and 50-69 years 174
TABLE 8.1. Key search teams for the review (not an exhaustive list) 261
TABLE 8.2. Typology to Classify a Country's Long-Term Care Services and Supports System 278
TABLE 9.1. Definition of long-term care by country 304
TABLE 9.2. Co-residency and long-term care provision among individuals ages 40 to 59 306
TABLE 9.3. Determinants of parental care, three-country pooled sample 308
TABLE 9.4. Labor supply among individuals ages 40 to 59 309
TABLE 9.5. Correlational effect on employment of providing long-term care to parents, by gender, four-country pooled sample 312
TABLE 9.6. Gender difference in the effect on employment of providing long-term care to parents, four-country pooled sample 313
TABLE 9.7. Correlational effect of providing long-term care to parents on employment, by country 313
TABLE 9.8. Correlational effect on employment of care hours devoted to parents, pooled sample from three countries 315
TABLE 9.9. Heterogeneous effect of long-term care provision by education level, pooled sample from four countries 316
TABLE 9.10. Heterogeneous effect of long-term care provision by presence of children in household, pooled sample from four countries 317
TABLE 9.11. Sensitivity check: including the number of adult females/males in households 318
TABLE 9.12. Correlational effect on employment of the intensity of long-term care provision to parents, pooled sample from three countries 319
TABLE 10.1. Years gained in life expectancy and healthy life expectancy at birth, 1990-2017. Both sexes, by demographic group 332
TABLE 10.2. Reasons given by adults aged 60 years or older for not accessing health care services, by country income category 339
TABLE 10.3. Long-term care services by type 357
TABLE 11.1. Individual ADLs (Age 65+) 385
TABLE 11.2. Marginal Effects from Logistic Regressions of Having Difficulty/Needing Help with at Least One ADL 387
TABLE 11.3. Individual IADLs (Age 65+) 389
TABLE 11.4. Marginal Effects from Logistic Regressions of Having Difficulty/Needing Help with at Least One IADL 390
TABLE 11.5. Linear Regressions of Count of Cumulative ADL & IADL Difficulties/Help Needs 392
TABLE 11.6. Marginal Effects from Logistic models of receiving any care (Age 65+ having difficulty with an ADL or IADL) 395
TABLE 11.7. Marginal Effects From Logistic models of receiving formal care (Age 65+ having difficulty with an ADL or IADL) 396
TABLE 12.1. Total number of studies by countries + characteristics of 8 countries which produced the highest number of studies 417
TABLE 12.2. Frequencies of risk factors studied in included studies 417
TABLE 12.3. Frequencies of outcomes identified in included studies 417
TABLE 12.4. Frequency of studies associated with different combinations of exposures and outcomes 418
TABLE 14.1. Design and scope of non-contributory programs targeted to the elderly 461
TABLE 14.2. Additional dimensions to identify factors to incorporate in the concept of adequacy pensions 467
TABLE 14.3. Comparison of average shares of OOP health expenditure between households with elderly in the poorest quintile versus households with elderly... 471
TABLE 15.1. Interventions considered in this chapter 478
TABLE 15.2. Cost and impact of all NCD interventions by 2050, by world region 479
TABLE 15.3. Value for money among interventions outside the health sector 481
TABLE 15.4. Non-cost-effectiveness criteria for prioritizing clinical interventions 482
TABLE 15.5. Cost and impact of locally tailored high-priority NCD packages, by world region 484
TABLE 15.6. Total cost per capita for priority NCD interventions by year and country income group 485
TABLE 15.7. Workforce and facility requirements for implementing the high-priority NCD package by 2050 485
TABLE 16.1. Bi-directional relationship between selected non-health sectors and NCDs - some illustrations 504
TABLE 16.2. NCD Control and Prevention System in Japan 513
TABLE 16.3. Major NCD Management Initiatives in China 514
TABLE 16.4. WBG IPF Operations with a 〉50 percent focus on NCDs 520
TABLE 16.5. DPL operations relevant to NCDs supported by the World Bank Group, 2009-2019 523
TABLE 17.1. Key actions and related domains when developing a healthy longevity dashboard 537
TABLE 17.2. Healthy longevity dashboard indicators for Sierra Leone, India, and Colombia 538
TABLE 17.3. Data ecosystem features by domain and information infrastructure maturity level 545
TABLE 17.4. Proposed healthy longevity indicators by information infrastructure maturity level 546
TABLE 17.5. Key dashboard users, their purpose, and types of measures needed by users 547
TABLE 18.1. Key actions and related domains when developing a healthy longevity dashboard 563
TABLE 18.2. Indicator domains and indicators in the HLI dashboard for setting with moderate data infrastructure, and data sources for the India HLI dashboard 565
TABLE 18.3. Indicators of context- India, lower-middle income countries and world in 2019 567
TABLE 18.4. HLI health indicators (domains 1-6) and scores based on percentile rank approach (P) and z-score approach (Z) for India 568
TABLE 18.5. HLI social and economic indicators (domains 7-10) and scores based on percentile rank approach (P) and z-score approach (Z) for India 570
FIGURE 1.1. GDP and GDP per capita gains, average for 10 countries, with an NCD package 49
FIGURE 1.2. GDP with (perturbed) and without (projected) an NCD package 49
FIGURE 1.3. Illustration of the theoretical model in terms of individual optimizing behavior 51
FIGURE 1.4. Estimated health capital per capita (logarithmic scale), for 92 countries, 2011 US$ PPP 52
FIGURE 1.5. Effect of NCDs on health capital and health investment 53
FIGURE 1.6. Worsening adult male mortality in former Soviet states, 1950-2000 57
FIGURE 1.7. Substantial NCD burdens among children in low- and middle-income countries 62
FIGURE 1.8. Trends in the risk of dying between ages 50 and 69 in 25 countries, 1970-2010 66
FIGURE 1.9. Framework for analyzing health research needs 67
FIGURE 2.1. Human capital life course trajectory 79
FIGURE 2.2. Impact channels between NCDs and inclusive growth 83
FIGURE 2.3. Impact channels between NCDs and human capital across the life cycle 86
FIGURE 3.1. Frontier mortality rates from 2000, 2019, and 2050 131
FIGURE 3.2. Avoidable mortality as percentage of total mortality, year 2019 132
FIGURE 3.3. Avoidable mortality globally and by region, year, and age group 134
FIGURE 3.4. Gap in life expectancy at birth between observed/projected life expectancy and frontier life expectancy 135
FIGURE 3.5. Ratio of average VSMU to initial VSMU, for United States age group 0-1 135
FIGURE 3.6. Value of avoidable mortality as percentage of annual income for years 2000, 2019, 2021, and 2050 (projected) 136
FIGURE 3.7. Relationship between avoidable mortality rate, GNI per capita, and value of avoidable mortality 137
FIGURE 3.8. Age-group contributions to the total value of avoidable mortality and population composition by age in year 2019 138
FIGURE 3.9. Value of avoidable mortality for females and males as percentage of annual income in year 2019 138
FIGURE 4.1. Mortality frontiers (females and males) for the period 2000-2050 152
FIGURE 4.2. Economic values of avoidable mortality 158
FIGURE 4.3. Rates of change (percent per year) of the economic values of avoidable mortality assigned to selected causes of death 159
FIGURE 5.1. Change in risk of death at start of age range, by age group and country income level, 1990-2019 165
FIGURE 5.2. Preston curve showing the relationship between life expectancy at birth and income (Preston 1975) 173
FIGURE 6.1. Conceptual model of traditional and behavioral determinants of NCDs and healthy aging 201
FIGURE 6.2. Example of specific biases affecting hypertension formation, detection, and management 203
FIGURE 8.1. Structure and Linkages for Women and Aging in Health Review 262
FIGURE 8.2. Cardiovascular Mortality among older adults by regional and income aggregates 264
FIGURE 8.3. Ratio of female to male CVD mortality by regional and income aggregates 264
FIGURE 8.4. Cardio-Vascular Disease by Sex for Older Populations (ages 45 years and above) 265
FIGURE 8.5. Deaths due to Diabetes, Ages 45+ (by Income Groups and Regional Aggregates) 266
FIGURE 8.6. Ratio of female to male mortality due to diabetes by regional and income aggregates 267
FIGURE 8.7. Gender Gaps in Diabetes for Older Populations (ages 45 years and above) 268
FIGURE 8.8. Deaths due to Cancers, Ages 45+ (by Income Groups and Regional Aggregates) 269
FIGURE 8.9. Ratio of female to male mortality due to cancers by regional and income aggregates 270
FIGURE 8.10. Gender Gaps in Cancers among Older Populations (ages 45 and above) 271
FIGURE 8.11. Gender Gaps in Depressive Disorders among Older Adults 272
FIGURE 8.12. Gender gaps in self-harm among older adults (ages 45 and above) 273
FIGURE 8.13. Breakdown of Health Expenditure per capita in PPP, 2019 279
FIGURE 8.14. Out of Pocket Expenditures, 2019 280
FIGURE 8.15. Share of female LTC workers in select OECD countries (% of total, latest available year) 284
FIGURE 9.1. Gross domestic product (GDP) per capita and male-female labor force participation gap, four countries, 2013-2018 302
FIGURE 9.2. Share of individuals (ages 25 to 59) with a coresident parent and young children in the household 307
FIGURE 10.1. Population by broad age group (thousands), estimates 1950-2020 and projections 2025-2100 330
FIGURE 10.2. Years required or expected for the population share aged 65+ to rise from 7 percent to 14 percent 331
FIGURE 10.3. Healthy and unhealthy life expectancy at age 65 years, 1990 and 2017 332
FIGURE 10.4. Burden of disease, by disease type, 1990-2017 (% of total DALYs) 335
FIGURE 10.5. Percentage of countries that have a national strategy for chronic diseases and their risk factors, by demographic stage 344
FIGURE 10.6. Percentage of countries with policies that target main chronic diseases risk factors, by type of policies and country's demographic stage 346
FIGURE 10.7. Countries that have national dementia plans in place, and percentage of their populations aged 80 and above 351
FIGURE 10.8. Projected increase in health care expenditures due to demographic effects, 2010-2060 (in percentage points) 354
FIGURE 11.1. Having difficulty with any one ADL (Age 65+) 386
FIGURE 11.2. Needing help with any one ADL (Age 65+) 386
FIGURE 11.3. Having difficulty with any one IADL (Age 65+) 389
FIGURE 11.4. Needing help with any one IADL (Age 65+) 389
FIGURE 11.5. Average number of cumulative ADL & IADL difficulties (Age 65+ having difficulty with an ADL or IADL) 392
FIGURE 11.6. Average number of cumulative ADL & IADL needs (Age 65+ needing help with an ADL or IADL) 392
FIGURE 11.7. Care mix (Age 65+ having difficulty with an ADL or IADL) 394
FIGURE 12.1. PRISMA flow diagram in search and selection of records 415
FIGURE 12.2. Proportion of studies by World Bank Regions (World Bank 2022) 416
FIGURE 12.3. Differences in outcomes identified by biological sex 420
FIGURE 13.1. Demographic changes differ across regions, but aging is coming everywhere 430
FIGURE 13.2. Labor force participation for older workers falls with a country's income 431
FIGURE 13.3. Labor force participation patterns are similar over the life cycle across richer and poorer countries 431
FIGURE 13.4. In MICs, pension coverage remains low 432
FIGURE 13.5. Healthy life expectancy has been increasing across the globe 434
FIGURE 13.6. A policy framework for longer and more productive working lives 436
FIGURE 13.7. Participation in formal or non-formal training, by age 439
FIGURE 13.8. Access to training through employers is limited, especially in LMICs 441
FIGURE 14.1. Coverage of non-contributory pensions, % population 65+ 463
FIGURE 14.2. Old age social pension beneficiaries, % population 65+ 463
FIGURE 14.3. Benefit amount, % GDP per capita 465
FIGURE 14.4. Expenditure on non-contributory pensions, % GDP (latest year) 466
FIGURE 14.5. Projected share of 60+ in total population in SAR 466
FIGURE 14.6. Out-of-pocket expenditure (% of current health expenditure) 471
FIGURE 14.7. Average share of out of pocket health expenditure by quintile and presence of persons age 65+ 472
FIGURE 15.1. Cost per DALY averted for 24 clinical interventions, by health system type 480
FIGURE 15.2. Final prioritization of NCD interventions, by health system type 483
FIGURE 15.3. Contribution of NCD interventions towards avoidable all-cause mortality 486
FIGURE 16.1. Trend in global deaths and disease burden by major cause (annual rate, 1990-2019) 493
FIGURE 16.2. Trend in deaths and disease burden by major cause in LMICs (annual rate, 1990-2019) 494
FIGURE 16.3. Global Deaths Attributed to Major Risk Factors, by sex, 2019 495
FIGURE 16.4. Global disease burden from NCDs by age, 1990 to 2019 496
FIGURE 16.5. Components of a "whole-of-society" approach 501
FIGURE 16.6. Framework for multisector causation and impact of non-communicable diseases 504
FIGURE 16.7. Global policy actions relevant to sugar-sweetened beverages 510
FIGURE 16.8. Singapore's Healthy Living Master Plan 515
FIGURE 16.9. Singapore's "War on Diabetes" 516
FIGURE 16.10. Thailand's ThaiHealth Program 517
FIGURE 16.11. World Bank investment lending for NCDs between FY16 and FY20 519
FIGURE 17.1. Healthy Longevity Initiative conceptual framework of human capital (HC) across the life course 536
FIGURE 17.2. Criteria for selecting healthy longevity indicators 537
FIGURE 18.1. Criteria and process of indicator selection 564
Boxes
BOX 1.1. Key messages 46
BOX 8.1. Gender gaps and the life course 260
BOX 8.2. The Healthy Longevity Framework and Gender 261
BOX 8.3. Understanding Long-Term Care Arrangements 278
BOX 8.4. Provider behaviors and access to care for older adults 281
BOX 8.5. Improving Quality of Care through Standards and Practice in the OECD 282
BOX 10.1. When is a country "aging"? 331
BOX 10.2. Health and socioeconomic status 339
BOX 10.3. How is functional dependency measured? 355
BOX 10.4. The importance of timely and sound data 371
BOX 11.1. Data used for the demand side analysis 384
BOX 16.1. Rationale for WoS approach - a sample of arguments 503
BOX 16.2. Examples of Public-Private Partnerships for Non-Communicable Diseases 508
BOX 16.3. Clínicas del Azúcar: a retail approach to diabetes care 523
BOX 16.4. Georgia Healthcare Group: universal health care delivered through the private sector 524
BOX 17.1. Case study of a healthy longevity dashboard in Sierra Leone 540
BOX 17.2. Case study of a healthy longevity dashboard in India 542
BOX 17.3. Case study of a healthy longevity dashboard in Colombia 543
Maps
MAP 14.1. High shares of informality in developing countries 468
MAP 14.2. Global Aging in 2020 469
MAP 14.3. Global Aging in 2050 469
Spotlights
SPOTLIGHT 13.1. Ok, Boomer! The aging brain and implications for work 436
SPOTLIGHT 13.2. Gray matter - training for the aging brain 445
SPOTLIGHT 13.3. Individual learning accounts to foster adult learning 446
SPOTLIGHT 13.4. Generation - facilitating labor market transitions over the working life 446
SPOTLIGHT 13.5. Firms with age-sensitive management practices 449
Annex Tables
TABLE 2A.1. Mapping the human capital trajectory and its interactions with ncds across the life cycle 120
TABLE 2A.2. Selected policies for human capital and ncds across the life course 121
TABLE 2A.3. Human capital promoting policies during working life for accumulation, deployment and protection of HC 123
TABLE 5A.1. Results of the hierarchical model predicting levels of mortality, by age and sex 178
TABLE 5A.2. Performance rankings of 71 LMICs in the rate of decline of mortality, by age and sex: 2000-10 and 2010-19 179
TABLE 5A.3. Change in performance in the annual rate of decline in mortality under 15 years, 15-49 years, 50-69 years, and 70-84 years, by sex from 2000-10... 187
TABLE 5A.4. Deaths avertable globally in 2019 from specific causes of deaths and age groups if rate of decline was same as that from HIV/AIDS (ages 0-14, 15-49)... 195
TABLE 6A.1. Summary of Behavioral Economics Concepts 226
TABLE 9A.1. Correlational effect on employment of providing long-term care to parents 321
TABLE 9A.2. Gender difference in the effect on employment of providing long-term care to parents 322
TABLE 12A.1. Search strategy for Ovid (MEDLINE) Sample 425
TABLE 13A.1. Labor market data for older adults 458
TABLE 17A.1. Available Data to Better Understand Population Ageing 560
TABLE 18A.1. List of 33 lower-middle income countries with population of more than 7 million in 2020 573
TABLE 18A.2. Indicator data sources for the HLI India dashboard 573
Annex Figures
FIGURE 5A.1. Schematic representation of an interrupted time series analysis 175
FIGURE 5A.2. Mortality rate, global and by country income level, by age and sex, between 2000 and 2019 176
FIGURE 5A.3. Correlation between performance in mortality decline during 2010-19 among males and females 187
FIGURE 8A.1. Cancer Mortality by Type, Ages 45+ years 298
FIGURE 8A.2. Prevalence of Cancer by Type, Ages 45+ years 299
FIGURE 9A.1. Kernel density of long-term care provision by age and country 323
FIGURE 9A.2. Work hours and care hours gradient 324
FIGURE 9A.3. Correlation between time spent on long-term care and employment 324
FIGURE 9A.4. Correlational effect of providing long-term care on individual employment by choice of control group 325
FIGURE 9A.5. Correlational effect of providing long-term care on annual earnings by choice of control group 325
FIGURE 9A.6. Correlational effect of providing long-term care on work hours by choice of control group 326
FIGURE 17A.1a. Polio transition program monitoring and evaluation dashboard 552
FIGURE 17A.1b. Polio transition program monitoring and evaluation dashboard 553
FIGURE 17A.2. Global Malaria Dashboard - Campaign Dashboard 554
FIGURE 17A.3. Global Malaria Dashboard - Supply Chain Dashboard 555
FIGURE 17A.4. Page 1 of The Countdown Country Profile: A Tool For Action for Colombia 556
FIGURE 17A.5. Section of the Child Health and Well-being Dashboard 557
FIGURE 17A.6. Climate Action Tracker dashboard for Canada 558
FIGURE 17A.7. Section of the Open SDG Data Hub Country Profile: India 559
*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
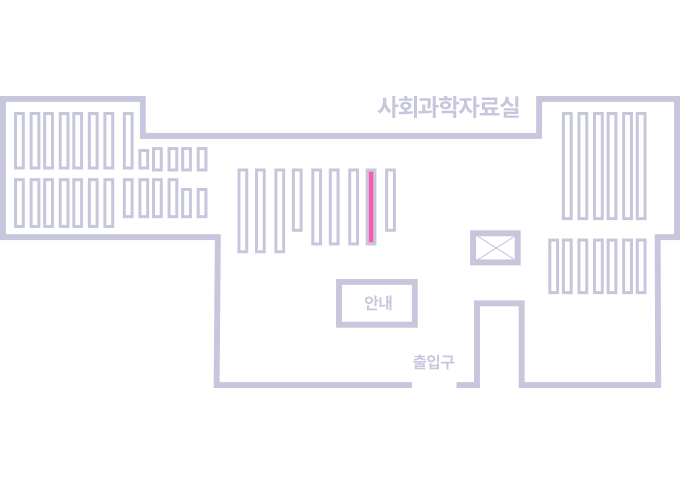
도서위치안내: / 서가번호:
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.