권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
| 번호 | 참고문헌 | 국회도서관 소장유무 |
|---|---|---|
| 1 | Marin RS. Apathy: a neuropsychiatric syndrome. J Neuropsychiatry Clin Neurosci 1991;3:243-254. | 미소장 |
| 2 | Robert P, Lanctôt KL, Agüera-Ortiz L, Aalten P, Bremond F, Defrancesco M, et al. Is it time to revise the diagnostic criteria for apathy in brain disorders? The 2018 international consensus group. Eur Psychiatry 2018;54:71-76. | 미소장 |
| 3 | Chong TT, Husain M. The role of dopamine in the pathophysiology and treatment of apathy. Prog Brain Res 2016;229:389-426. | 미소장 |
| 4 | van Reekum R, Stuss DT, Ostrander L. Apathy: why care? J Neuropsychiatry Clin Neurosci 2005;17:7-19. | 미소장 |
| 5 | Husain M, Roiser JP. Neuroscience of apathy and anhedonia:a transdiagnostic approach. Nat Rev Neurosci 2018;19:470-484. | 미소장 |
| 6 | van der Linde RM, Matthews FE, Dening T, Brayne C. Patterns and persistence of behavioural and psychological symptoms in those with cognitive impairment: the importance of apathy. Int J Geriatr Psychiatry 2017;32:306-315. | 미소장 |
| 7 | Massimo L, Evans LK. Differentiating subtypes of apathy to improve person-centered care in frontotemporal degeneration. J Gerontol Nurs 2014;40:58-65. | 미소장 |
| 8 | Pardini M, Cordano C, Guida S, Grafman J, Krueger F, Sassos D, et al. Prevalence and cognitive underpinnings of isolated apathy in young healthy subjects. J Affect Disord 2016;189:272-275. | 미소장 |
| 9 | Brodaty H, Altendorf A, Withall A, Sachdev P. Do people become more apathetic as they grow older? A longitudinal study in healthy individuals. Int Psychogeriatr 2010;22:426-436. | 미소장 |
| 10 | Nobis L, Husain M. Apathy in Alzheimer’s disease. Curr Opin Behav Sci 2018;22:7-13. | 미소장 |
| 11 | Radakovic R, Abrahams S. Multidimensional apathy: evidence from neurodegenerative disease. Curr Opin Behav Sci 2018;22:42-49. | 미소장 |
| 12 | Rizvi SJ, Pizzagalli DA, Sproule BA, Kennedy SH. Assessing anhedonia in depression: potentials and pitfalls. Neurosci Biobehav Rev 2016;65:21-35. | 미소장 |
| 13 | Kano M, Fukudo S. The alexithymic brain: the neural pathways linking alexithymia to physical disorders. Biopsychosoc Med 2013;7:1. | 미소장 |
| 14 | Le Heron C, Apps MAJ, Husain M. The anatomy of apathy: a neurocognitive framework for amotivated behaviour. Neuropsychologia 2018;118(Pt B):54-67. | 미소장 |
| 15 | Huey ED, Lee S, Cheran G, Grafman J, Devanand DP. Brain regions brain regions involved in arousal and reward processing are associated with apathy in Alzheimer’s disease and frontotemporal dementia. J Alzheimers Dis 2017;55:551-558. | 미소장 |
| 16 | Gard DE, Kring AM, Gard MG, Horan WP, Green MF. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr Res 2007;93:253-260. | 미소장 |
| 17 | Kringelbach ML. The human orbitofrontal cortex: linking reward to hedonic experience. Nat Rev Neurosci 2005;6:691-702. | 미소장 |
| 18 | Berns GS, McClure SM, Pagnoni G, Montague PR. Predictability modulates human brain response to reward. J Neurosci 2001;21:2793-2798. | 미소장 |
| 19 | Simon JJ, Biller A, Walther S, Roesch-Ely D, Stippich C, Weisbrod M, et al. Neural correlates of reward processing in schizo-phrenia--relationship to apathy and depression. Schizophr Res 2010;118:154-161. | 미소장 |
| 20 | Steffens DC, Krishnan KR. Structural neuroimaging and mood disorders: recent findings, implications for classification, and future directions. Biol Psychiatry 1998;43:705-712. | 미소장 |
| 21 | Alexopoulos GS. Frontostriatal and limbic dysfunction in late-life depression. Am J Geriatr Psychiatry 2002;10:687-695. | 미소장 |
| 22 | Cieri F, Esposito R, Cera N, Pieramico V, Tartaro A, di Giannantonio M. Late-life depression: modifications of brain resting state activity. J Geriatr Psychiatry Neurol 2017;30:140-150. | 미소장 |
| 23 | Tadayonnejad R, Yang S, Kumar A, Ajilore O. Multimodal brain connectivity analysis in unmedicated late-life depression. PLoS One 2014;9:e96033. | 미소장 |
| 24 | Aizenstein HJ, Butters MA, Wu M, Mazurkewicz LM, Stenger VA, Gianaros PJ, et al. Altered functioning of the executive control circuit in late-life depression: episodic and persistent phenomena. Am J Geriatr Psychiatry 2009;17:30-42. | 미소장 |
| 25 | Brassen S, Kalisch R, Weber-Fahr W, Braus DF, Büchel C. Ventromedial prefrontal cortex processing during emotional evaluation in late-life depression: a longitudinal functional magnetic resonance imaging study. Biol Psychiatry 2008;64:349-355. | 미소장 |
| 26 | Starkstein SE, Fedoroff JP, Price TR, Leiguarda R, Robinson RG. Apathy following cerebrovascular lesions. Stroke 1993;24:1625-1630. | 미소장 |
| 27 | Tay J, Lisiecka-Ford DM, Hollocks MJ, Tuladhar AM, Barrick TR, Forster A, et al. Network neuroscience of apathy in cerebrovascular disease. Prog Neurobiol 2020;188:101785. | 미소장 |
| 28 | Jang SH, Kim SH, Kwon HG. Injury of the prefronto-caudate tract in a patient with apathy following intracerebral hemorrhage in the caudate nucleus. Acta Neurol Belg 2019;119:143-145. | 미소장 |
| 29 | Hollocks MJ, Lawrence AJ, Brookes RL, Barrick TR, Morris RG, Husain M, et al. Differential relationships between apathy and depression with white matter microstructural changes and functional outcomes. Brain 2015;138(Pt 12):3803-3815. | 미소장 |
| 30 | Tuladhar AM, Tay J, van Leijsen E, Lawrence AJ, van Uden IWM, Bergkamp M, et al. Structural network changes in cerebral small vessel disease. J Neurol Neurosurg Psychiatry 2020;91:196-203. | 미소장 |
| 31 | Padala PR, Padala KP, Lensing SY, Jackson AN, Hunter CR, Parkes CM, et al. Repetitive transcranial magnetic stimulation for apathy in mild cognitive impairment: a double-blind, randomized, sham-controlled, cross-over pilot study. Psychiatry Res 2018;261:312-318. | 미소장 |
| 32 | Lyketsos CG, Steinberg M, Tschanz JT, Norton MC, Steffens DC, Breitner JC. Mental and behavioral disturbances in dementia: findings from the Cache County Study on Memory in Aging. Am J Psychiatry 2000;157:708-714. | 미소장 |
| 33 | Kim JW, Lee DY, Choo IH, Seo EH, Kim SG, Park SY, et al. Microstructural alteration of the anterior cingulum is associated with apathy in Alzheimer disease. Am J Geriatr Psychiatry 2011;19:644-653. | 미소장 |
| 34 | Mendez MF, Lauterbach EC, Sampson SM. An evidencebased review of the psychopathology of frontotemporal dementia: a report of the ANPA Committee on Research. J Neuropsychiatry Clin Neurosci 2008;20:130-149. | 미소장 |
| 35 | Rosen HJ, Allison SC, Schauer GF, Gorno-Tempini ML, Weiner MW, Miller BL. Neuroanatomical correlates of behavioural disorders in dementia. Brain 2005;128(Pt 11):2612-2625. | 미소장 |
| 36 | Sarazin M, Michon A, Pillon B, Samson Y, Canuto A, Gold G, et al. Metabolic correlates of behavioral and affective disturbances in frontal lobe pathologies. J Neurol 2003;250:827-833. | 미소장 |
| 37 | Liu J, Cooper CA, Weintraub D, Dahodwala N. Pharmacological treatment of apathy in Lewy body disorders: a systematic review. Parkinsonism Relat Disord 2019;60:14-24. | 미소장 |
| 38 | Pagonabarraga J, Kulisevsky J, Strafella AP, Krack P. Apathy in Parkinson’s disease: clinical features, neural substrates, diagnosis, and treatment. Lancet Neurol 2015;14:518-531. | 미소장 |
| 39 | Radakovic R, Abrahams S. Developing a new apathy measurement scale: Dimensional Apathy Scale. Psychiatry Res 2014;219:658-663. | 미소장 |
| 40 | Sockeel P, Dujardin K, Devos D, Denève C, Destée A, Defebvre L. The Lille apathy rating scale (LARS), a new instrument for detecting and quantifying apathy: validation in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2006;77:579-584. | 미소장 |
| 41 | Ang YS, Lockwood P, Apps MA, Muhammed K, Husain M. Distinct subtypes of apathy revealed by the apathy motivation index. PLoS One 2017;12:e0169938. | 미소장 |
| 42 | Theleritis C, Politis A, Siarkos K, Lyketsos CG. A review of neuroimaging findings of apathy in Alzheimer’s disease. Int Psychogeriatr 2014;26:195-207. | 미소장 |
| 43 | Theleritis C, Siarkos K, Politis AA, Katirtzoglou E, Politis A. A systematic review of non-pharmacological treatments for apathy in dementia. Int J Geriatr Psychiatry 2018;33:e177-e192. | 미소장 |
| 44 | Yuen GS, Gunning FM, Woods E, Klimstra SA, Hoptman MJ, Alexopoulos GS. Neuroanatomical correlates of apathy in late-life depression and antidepressant treatment response. J Affect Disord 2014;166:179-186. | 미소장 |
| 45 | Moretti R, Torre P, Antonello RM, Cazzato G, Bava A. Rivastigmine in subcortical vascular dementia: an open 22-month study. J Neurol Sci 2002;203-204:141-146. | 미소장 |
| 46 | Rea R, Carotenuto A, Fasanaro AM, Traini E, Amenta F. Apathy in Alzheimer’s disease: any effective treatment? ScientificWorldJournal 2014;2014:421385. | 미소장 |
| 47 | Rea R, Carotenuto A, Traini E, Fasanaro AM, Manzo V, Amenta F. Apathy treatment in Alzheimer’s disease: interim results of the ASCOMALVA trial. J Alzheimers Dis 2015;48:377-383. | 미소장 |
| 48 | Padala PR, Padala KP, Lensing SY, Ramirez D, Monga V, Bopp MM, et al. Methylphenidate for apathy in community-dwell-ing older veterans with mild Alzheimer’s disease: a doubleblind, randomized, placebo-controlled trial. Am J Psychiatry 2018;175:159-168. | 미소장 |
| 49 | Takemoto M, Ohta Y, Hishikawa N, Yamashita T, Nomura E, Tsunoda K, et al. The efficacy of sertraline, escitalopram, and nicergoline in the treatment of depression and apathy in Alzheimer’s disease: the Okayama Depression and Apathy Project (ODAP). J Alzheimers Dis 2020;76:769-772. | 미소장 |
| 50 | Pérez-Pérez J, Pagonabarraga J, Martínez-Horta S, FernándezBobadilla R, Sierra S, Pascual-Sedano B, et al. Head-to-head comparison of the neuropsychiatric effect of dopamine agonists in Parkinson’s disease: a prospective, cross-sectional study in non-demented patients. Drugs Aging 2015;32:401-407. | 미소장 |
| 51 | Overvliet GM, Vlaar A, de Haan C, Lampe I. Pharmacological treatment of apathy in Parkinson’s disease, review of the literature. Parkinsonism Relat Disord 2020;79(Suppl 1):E70-E71. | 미소장 |
| 52 | Moretti R, Caruso P, Dal Ben M. Rivastigmine as a symptomatic treatment for apathy in Parkinson’s dementia complex:new aspects for this riddle. Parkinsons Dis 2017;2017:6219851. | 미소장 |
| 53 | Zahodne LB, Bernal-Pacheco O, Bowers D, Ward H, Oyama G, Limotai N, et al. Are selective serotonin reuptake inhibitors associated with greater apathy in Parkinson’s disease? J Neuropsychiatry Clin Neurosci 2012;24:326-330. | 미소장 |
| 54 | Callegari I, Mattei C, Benassi F, Krueger F, Grafman J, Yaldizli Ö, et al. Agomelatine improves apathy in frontotemporal dementia. Neurodegener Dis 2016;16:352-356. | 미소장 |
| 55 | Herrmann N, Black SE, Chow T, Cappell J, Tang-Wai DF, Lanctôt KL. Serotonergic function and treatment of behavioral and psychological symptoms of frontotemporal dementia. Am J Geriatr Psychiatry 2012;20:789-797. | 미소장 |
| 56 | Finger E, Berry S, Cummings J, Coleman K, Hsiung R, Feldman HH, et al. Adaptive crossover designs for assessment of symptomatic treatments targeting behaviour in neurodegenerative disease: a phase 2 clinical trial of intranasal oxytocin for frontotemporal dementia (FOXY). Alzheimers Res Ther 2018;10:102. | 미소장 |
*표시는 필수 입력사항입니다.
| *전화번호 | ※ '-' 없이 휴대폰번호를 입력하세요 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
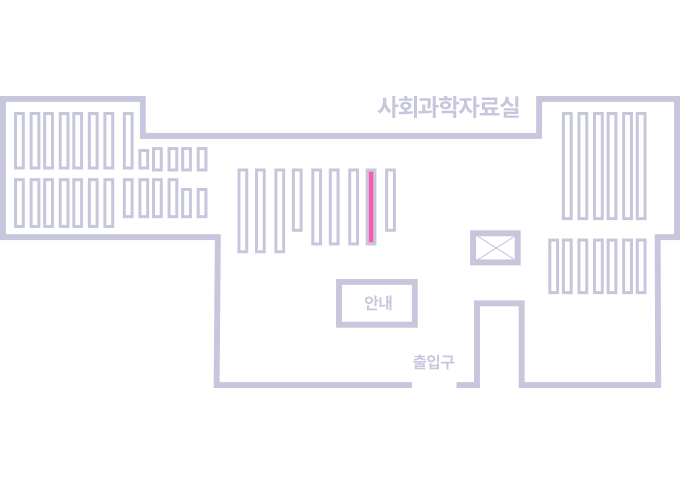
도서위치안내: 정기간행물실(524호) / 서가번호: 국내16
2021년 이전 정기간행물은 온라인 신청(원문 구축 자료는 원문 이용)
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.