권호기사보기
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 대표형(전거형, Authority) | 생물정보 | 이형(異形, Variant) | 소속 | 직위 | 직업 | 활동분야 | 주기 | 서지 | |
|---|---|---|---|---|---|---|---|---|---|
| 연구/단체명을 입력해주세요. | |||||||||
|
|
|
|
|
|
* 주제를 선택하시면 검색 상세로 이동합니다.
| 기사명 | 저자명 | 페이지 | 원문 | 목차 |
|---|---|---|---|---|
| Clinical practice guideline for percutaneous endoscopic gastrostomy | Chung Hyun Tae, Ju Yup Lee, Moon Kyung Joo, Chan Hyuk Park, Eun Jeong Gong, Cheol Min Shin, Hyun Lim, Hyuk Soon Choi, Miyoung Choi, Sang Hoon Kim ... [et al.] | p. 10-26 |
|
|
| Recent advances in the pathogenesis and clinical evaluation of portal hypertension in chronic liver disease | Kohei Kotani, Norifumi Kawada | p. 27-39 |
|
|
| Delayed perforation occurring after gastric endoscopic submucosal dissection : clinical features and management strategy | Tae-Se Kim, Byung-Hoon Min, Yang Won Min, Hyuk Lee, Poong-Lyul Rhee, Jae J. Kim, Jun Haeng Lee | p. 40-49 |
|
|
| Mucosal and submucosal thickening of esophageal wall is a promising factor in the development of symptoms in eosinophilic esophagitis | Yugo Suzuki, Yorinari Ochiai, Atsuko Hosoi, Takayuki Okamura, Junnosuke Hayasaka, Yutaka Mitsunaga, Masami Tanaka, Hiroyuki Odagiri, Kosuke Nomura, Satoshi Yamashita, Akira Matsui, Daisuke Kikuchi, Kenichi Ohashi, Shu Hoteya | p. 50-59 |
|
|
| Utilization of an automated latex agglutination turbidity assay for assessing gastric mucosal alteration during helicobacter pylori infection | Ayush Khangai, Junko Akada, Batsaikhan Saruuljavkhlan, Boldbaatar Gantuya, Dashdorj Azzaya, Khasag Oyuntsetseg, Duger Davaadorj, Tomohisa Uchida, Takashi Matsumoto, Yoshio Yamaoka | p. 60-69 |
|
|
| Evaluation of the efficacy and safety of DW1903 in patients with gastritis : a randomized, double-blind, noninferiority, multicenter, phase 3 study | Jie-Hyun Kim, Hwoon-Yong Jung, In Kyung Yoo, Seon-Young Park, Jae Gyu Kim, Jae Kyu Sung, Jin Seok Jang, Gab Jin Cheon, Kyoung Oh Kim, Tae Oh Kim ... [et al.] | p. 70-76 |
|
|
| (A) multicenter survey of percutaneous endoscopic gastrostomy in 2019 at Korean medical institutions | Jun Woo Park, Tae Gyun Kim, Kwang Bum Cho, Jeong Seok Kim, Jin Woong Cho, Jung Won Jeon, Sun Gyo Lim, Chan Gyoo Kim, Hong Jun Park, Tae Jun Kim, Eun Sun Kim, Su Jin Jeong, Yong Hwan Kwon, The Research for Multidisciplinary Therapeutic Endoscopy group of Korean Society of Gastrointestinal Endoscopy | p. 77-84 |
|
|
| Surgical options for appropriate length of J-pouch construction for better outcomes and long-term quality of life in patients with ulcerative colitis after ileal pouch-anal anastomosis | Weimin Xu, Wenbo Tang, Wenjun Ding, Zhebin Hua, Yaosheng Wang, Xiaolong Ge, Long Cui, Xiaojian Wu, Wei Zhou, Zhao Ding, Peng Du | p. 85-96 |
|
|
| Comparison of an endoscopic scoring system and the simplified magnetic resonance index of activity in patients with small bowel Crohn’s disease | Ji Eun Na, Hon Soul Kim, Sung Noh Hong, Kyoung Doo Song, Ji Eun Kim, Eun Ran Kim, Young-Ho Kim, Dong Kyung Chang | p. 97-105 |
|
|
| Factors associated with reaching mid-parental height in patients diagnosed with inflammatory bowel disease in childhood and adolescent period | So Yoon Choi, Sujin Choi, Byung-Ho Choe, Jae Hong Park, Kwang-Hae Choi, Hae Jeong Lee, Ji Sook Park, Ji-Hyun Seo, Jae Young Kim, Hyo-Jeong Jang, Suk Jin Hong, Eun Young Kim, Yeoun Joo Lee, Ben Kang | p. 106-115 |
|
|
| Sorafenib for 9,923 patients with hepatocellular carcinoma : an analysis from national health insurance claim data in South Korea | Sojung Han, Do Young Kim, Ho Yeong Lim, Jung-Hwan Yoon, Baek-Yeol Ryoo, Yujeong Kim, Kookhee Kim, Bo Yeon Kim, So Young Yi, Dong-Sook Kim, Do-Yeon Cho, Jina Yu, Suhyun Kim, Joong-Won Park | p. 116-124 |
|
|
| Chemoembolization versus radiotherapy for single hepatocellular carcinomas of ≤3 cm unsuitable for image-guided tumor ablation | Jihye Lim, Euichang Kim, Sehee Kim, So Yeon Kim, Jin Hyoung Kim, Sang Min Yoon, Ju Hyun Shim | p. 125-134 |
|
|
| Cost-utility analysis of non-contrast abbreviated magnetic resonance imaging for hepatocellular carcinoma surveillance in cirrhosis | Pakanat Decharatanachart, Wirichada Pan-ngum, Thoetchai Peeraphatdit, Natthaporn Tanpowpong, Pisit Tangkijvanich, Sombat Treeprasertsuk, Rungsun Rerknimitr, Roongruedee Chaiteerakij | p. 135-146 |
|
|
| Prediction of hepatocellular carcinoma development in Korean patients after hepatitis C cure with direct-acting antivirals | Hyeyeon Hong, Won-Mook Choi, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jonggi Choi | p. 147-155 |
|
|
| Reappraisal of portal vein tumor thrombosis as a prognostic factor for patients with hepatocellular carcinoma | Young Chang, Su Jong Yu, Hyo-Cheol Kim, Yun Bin Lee, Eun Ju Cho, Jeong-Hoon Lee, Yoon Jun Kim, Jin Wook Chung, Jung-Hwan Yoon | p. 156-164 |
|
|
| Clinical significance of venous thromboembolism in patients with advanced cholangiocarcinoma | Joo Seong Kim, Woo Hyun Paik, Sang Hyub Lee, Min Woo Lee, Namyoung Park, Jin Ho Choi, In Rae Cho, Ji Kon Ryu, Yong-Tae Kim | p. 165-173 |
|
|
| Diagnosis and treatment of perihilar cholangiocarcinoma : a national survey from the Korean Pancreatobiliary Association | Eunae Cho, Seong-Hun Kim, Seong Ji Choi, Min Kyu Jung, Byeong Jun Song, Jin Myung Park, Jingu Kang, Won Suk Park, Joo Kyung Park, Sang Myung Woo, Hyo Jung Kim, Study Group for Biliary Diseases, Korean Pancreatobiliary Association | p. 174-183 |
|
|
| Factors influencing the diagnostic performance of repeat endoscopic ultrasound-guided fine-needle aspiration/biopsy after the first inconclusive diagnosis of pancreatic solid lesions | Jae Hee Cho, Jaihwan Kim, Hee Seung Lee, Su Jeong Ryu, Sung Ill Jang, Eui Joo Kim, Huapyong Kang, Sang Soo Lee, Tae Jun Song, Seungmin Bang | p. 184-191 |
|
| 번호 | 참고문헌 | 국회도서관 소장유무 |
|---|---|---|
| 1 | Heuschkel R, Salvestrini C, Beattie RM, Hildebrand H, Walters T, Griffiths A. Guidelines for the management of growth failure in childhood inflammatory bowel disease. Inflamm Bowel Dis 2008;14:839-849. | 미소장 |
| 2 | Hildebrand H, Karlberg J, Kristiansson B. Longitudinal growth in children and adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 1994;18:165-173. | 미소장 |
| 3 | Turner D, Ricciuto A, Lewis A, et al. STRIDE-II: an update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) initiative of the International Organization for the Study of IBD (IOIBD). Determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology 2021;160:1570-1583. | 미소장 |
| 4 | Shamir R, Phillip M, Levine A. Growth retardation in pediatric Crohn's disease: pathogenesis and interventions. Inflamm Bowel Dis 2007;13:620-628. | 미소장 |
| 5 | Ley D, Duhamel A, Behal H, et al. Growth pattern in paediatric Crohn disease is related to inflammatory status. J Pediatr Gastroenterol Nutr 2016;63:637-643. | 미소장 |
| 6 | Alemzadeh N, Rekers-Mombarg LT, Mearin ML, Wit JM, Lamers CB, van Hogezand RA. Adult height in patients with early onset of Crohn's disease. Gut 2002;51:26-29. | 미소장 |
| 7 | Sawczenko A, Ballinger AB, Savage MO, Sanderson IR. Clinical features affecting final adult height in patients with pediatric-onset Crohn's disease. Pediatrics 2006;118:124-129. | 미소장 |
| 8 | Levine A, Koletzko S, Turner D, et al. ESPGHAN revised Porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 2014;58:795-806. | 미소장 |
| 9 | Levine A, Griffiths A, Markowitz J, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis 2011;17:1314-1321. | 미소장 |
| 10 | Hyams JS, Ferry GD, Mandel FS, et al. Development and validation of a pediatric Crohn's disease activity index. J Pediatr Gastroenterol Nutr 1991;12:439-447. | 미소장 |
| 11 | Turner D, Ruemmele FM, Orlanski-Meyer E, et al. Management of paediatric ulcerative colitis, part 1: ambulatory carean evidence-based guideline from European Crohn's and Colitis Organization and European Society of Paediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2018;67:257-291. | 미소장 |
| 12 | Tanner JM, Goldstein H, Whitehouse RH. Standards for children's height at ages 2-9 years allowing for heights of parents. Arch Dis Child 1970;45:755-762. | 미소장 |
| 13 | Kim JH, Yun S, Hwang SS, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr 2018;61:135-149. | 미소장 |
| 14 | Lee JJ, Escher JC, Shuman MJ, et al. Final adult height of children with inflammatory bowel disease is predicted by parental height and patient minimum height Z-score. Inflamm Bowel Dis 2010;16:1669-1677. | 미소장 |
| 15 | Koh SJ, Hong SN, Park SK, et al. Korean clinical practice guidelines on biologics for moderate to severe Crohn's disease. Intest Res 2023;21:43-60. | 미소장 |
| 16 | Na SY, Choi CH, Song EM, et al. Korean clinical practice guidelines on biologics and small molecules for moderateto-severe ulcerative colitis. Intest Res 2023;21:61-87. | 미소장 |
| 17 | Singh A, Mahajan R, Kedia S, et al. Use of thiopurines in inflammatory bowel disease: an update. Intest Res 2022;20:11-30. | 미소장 |
| 18 | Kang B, Choe YH. Early biologic treatment in pediatric Crohn's disease: catching the therapeutic window of opportunity in early disease by treat-to-target. Pediatr Gastroenterol Hepatol Nutr 2018;21:1-11. | 미소장 |
| 19 | Kang B, Choi SY, Kim HS, Kim K, Lee YM, Choe YH. Mucosal healing in paediatric patients with moderate-to-severe luminal Crohn's disease under combined immunosuppression:escalation versus early treatment. J Crohns Colitis 2016;10:1279-1286. | 미소장 |
| 20 | Burnham JM, Shults J, Semeao E, et al. Whole body BMC in pediatric Crohn disease: independent effects of altered growth, maturation, and body composition. J Bone Miner Res 2004;19:1961-1968. | 미소장 |
| 21 | Malik S, Wong SC, Bishop J, et al. Improvement in growth of children with Crohn disease following anti-TNF-α therapy can be independent of pubertal progress and glucocorticoid reduction. J Pediatr Gastroenterol Nutr 2011;52:31-37. | 미소장 |
| 22 | Newby EA, Sawczenko A, Thomas AG, Wilson D. Interventions for growth failure in childhood Crohn's disease. Cochrane Database Syst Rev 2005;2005:CD003873. | 미소장 |
| 23 | Sanderson IR, Udeen S, Davies PS, Savage MO, Walker-Smith JA. Remission induced by an elemental diet in small bowel Crohn's disease. Arch Dis Child 1987;62:123-127. | 미소장 |
| 24 | Connors J, Basseri S, Grant A, et al. Exclusive enteral nutrition therapy in paediatric Crohn's disease results in long-term avoidance of corticosteroids: results of a propensity-score matched cohort analysis. J Crohns Colitis 2017;11:1063-1070. | 미소장 |
| 25 | Cohen-Dolev N, Sladek M, Hussey S, et al. Differences in outcomes over time with exclusive enteral nutrition compared with steroids in children with mild to moderate Crohn's disease: results from the GROWTH CD study. J Crohns Colitis 2018;12:306-312. | 미소장 |
| 26 | Walters TD, Gilman AR, Griffiths AM. Linear growth improves during infliximab therapy in children with chronically active severe Crohn's disease. Inflamm Bowel Dis 2007;13:424-430. | 미소장 |
| 27 | Church PC, Guan J, Walters TD, et al. Infliximab maintains durable response and facilitates catch-up growth in luminal pediatric Crohn's disease. Inflamm Bowel Dis 2014;20:1177-1186. | 미소장 |
| 28 | Borrelli O, Bascietto C, Viola F, et al. Infliximab heals intestinal inflammatory lesions and restores growth in children with Crohn's disease. Dig Liver Dis 2004;36:342-347. | 미소장 |
| 29 | Choi J, Kang B, Kim MJ, Sohn I, Lee HJ, Choe YH. Early infliximab yields superior long-term effects on linear growth in pediatric Crohn's disease patients. Gut Liver 2018;12:255-262. | 미소장 |
| 30 | Walters TD, Faubion WA, Griffiths AM, et al. Growth improvement with adalimumab treatment in children with moderately to severely active Crohn's disease. Inflamm Bowel Dis 2017;23:967-975. | 미소장 |
| 31 | Varille V, Cézard JP, de Lagausie P, et al. Resting energy expenditure before and after surgical resection of gut lesions in pediatric Crohn's disease. J Pediatr Gastroenterol Nutr 1996;23:13-19. | 미소장 |
| 32 | Carmichael CM, McGue M. A cross-sectional examination of height, weight, and body mass index in adult twins. J Gerontol A Biol Sci Med Sci 1995;50:B237-B244. | 미소장 |
| 33 | Dubois L, Ohm Kyvik K, Girard M, et al. Genetic and environmental contributions to weight, height, and BMI from birth to 19 years of age: an international study of over 12,000twin pairs. PLoS One 2012;7:e30153. | 미소장 |
| 34 | Phillips K, Matheny AP Jr. Quantitative genetic analysis of longitudinal trends in height: preliminary results from the Louisville Twin Study. Acta Genet Med Gemellol (Roma)1990;39:143-163. | 미소장 |
*표시는 필수 입력사항입니다.
| 전화번호 |
|---|
| 기사명 | 저자명 | 페이지 | 원문 | 기사목차 |
|---|
| 번호 | 발행일자 | 권호명 | 제본정보 | 자료실 | 원문 | 신청 페이지 |
|---|
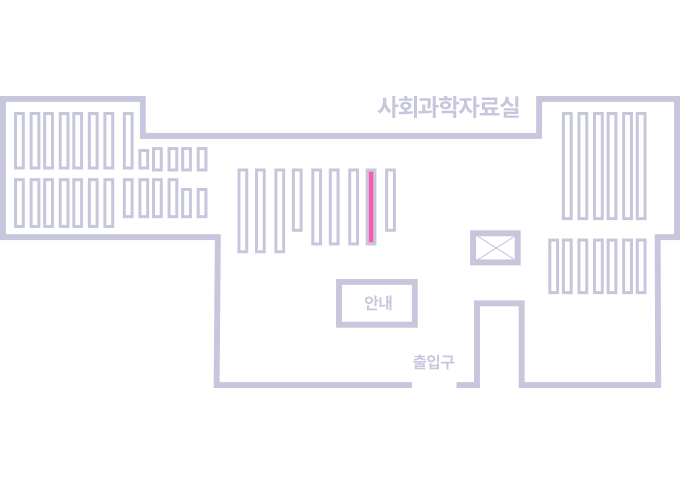
도서위치안내: 정기간행물실(524호) / 서가번호: 국내17
2021년 이전 정기간행물은 온라인 신청(원문 구축 자료는 원문 이용)
우편복사 목록담기를 완료하였습니다.
*표시는 필수 입력사항입니다.
저장 되었습니다.